9 February 2020
Researchers at the State University of New York recently uncovered a possible route to restoring the memory loss and other cognitive functions that are the distressing hallmark of Alzheimer’s1.
The results come mainly from investigations in mice and cultured human cells, but the researchers report that the insights in mice are now being matched by early work with human cells.
Their work focuses on changes in the regulation of the activity of key genes, rather than on the DNA sequence of the genes. Alzheimer’s has long been attributed to a mixture of genes that bestow susceptibility to the disease and subtler gene regulatory processes, known as epigenetics.
A common epigenetic control mechanism involves the addition of methyl groups (CH3) to proteins called histones that are bundled together with the DNA of chromosomes and control gene activity.
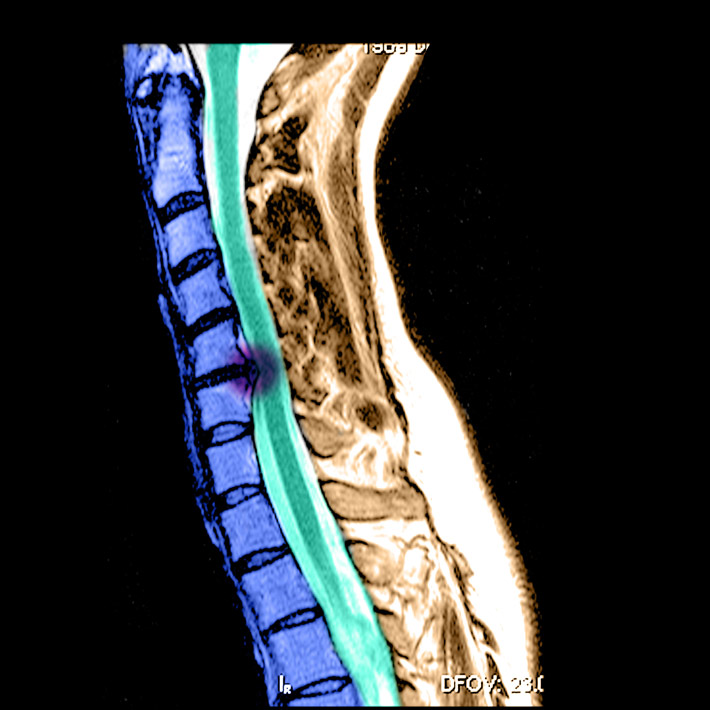
The researchers’ first key finding is that in mice with a form of Alzheimer’s this histone ‘methylation’ process significantly reduces the levels and activity of proteins required for the normal transmission of nerve impulses in the brain.
The proteins are receptors that sit in nerve cell membranes and bind to the neurotransmitter glutamate. Neurotransmitter molecules allow signals travelling along one nerve cell to influence the activity of other cells. This communication is the essence of how our brain cells work together to make our minds.
The damaging methylation revealed in the research is catalyzed by two proteins, EHMT1 and EHMT2, the elevated activity of which was detected in the brains of the Alzheimer’s mice. Examining post-mortem tissues from human patients also suggested increased methylation activity of the type catalyzed by EHMT1 and EHMT2. This forges a crucial link between the mouse studies and the human disease.
Rescuing memories
The researchers speculated that the key to treating this specific aspect of Alzheimer’s might be to inhibit the methylation. Fortunately, chemicals that inhibit the two implicated proteins were already known, allowing the possibility to be readily tested.
Injecting an inhibitor of EHMT1 and EHMT2 into affected mice achieved what the researchers describe as the ‘rescue’ of cognitive function, which was confirmed through tests of recognition memory, spatial memory and working memory. These included the ability of the mice to remember their way through mazes and to demonstrate recognition of previously encountered objects.
“We were quite surprised to see such dramatic cognitive improvement,” says Zhen Yan of the research team.
There is a long road to travel between preliminary results in a mouse model and the development, testing and approval of a treatment for humans. Nevertheless, a new door has been opened and the Buffalo research team are already developing the work further.
Yan reports that her team has conducted proof of concept trials in cultured human nerve cells, to confirm that the approach can lead to the recovery of signalling function in the human cells. She says that the “promising” results will be published soon.
“One of the most exciting aspects of epigenetic research is that the changes are potentially reversible,” says Jana Voigt, Head of Research at Alzheimer's Research UK, commenting on the paper. "These interesting findings in mice now need to be taken forward in studies in people, to explore whether they could form the basis of a future treatment,” Voigt concludes.
A link with oral bacteria
Looking back to the start of the trail of cause and effect in Alzheimer’s, researchers have recently uncovered surprising evidence that the disease may be linked to bacteria that cause gum disease2.
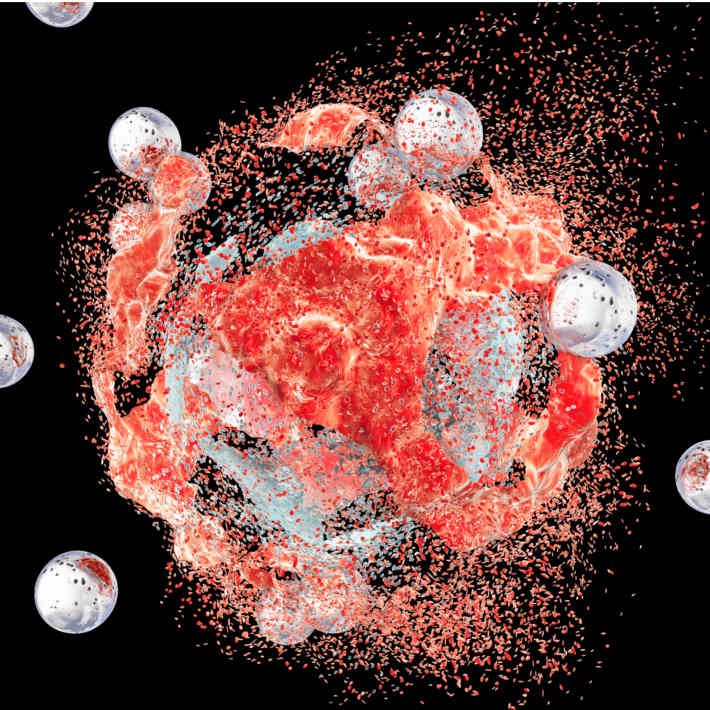
Research led by US biopharmaceutical company Cortexyme Inc. found Porphyromonas gingivalis, a bacterium associated with chronic gum disease, in post-mortem tissue from the brains of patients with Alzheimer’s. The researchers also found that the levels of this bacterial infection showed a correlation with those of two types of protein, called tau and ubiquitin, which malfunction and accumulate in the brain in Alzheimer’s disease. And when mice were infected with P. gingivalis the bacterium was found to colonize the brain alongside increased production of proteins that combine to form aggregates called amyloid plaques, which are strongly implicated in the damage found in Alzheimer’s-affected brains.
There was no evidence of the transport of two other common types of oral bacteria into the mouse brains, suggesting the link to Alzheimer’s may be limited to specific bacteria, or perhaps to P. gingivalis alone.
The bacterium itself produces toxic proteins called gingipains, and these were also found in the brain tissue of Alzheimer’s patients at levels that correlated with the tau and ubiquitin proteins.
“We believe P. gingivalis and its associated gingipains cause the majority of what is currently being diagnosed as Alzheimer's disease,” says Stephen Dominy of the Cortexyme team. If confirmed, that would surely be a startling advance in understanding.
One obvious possible significance of the bacterial link is that poor oral hygiene may increase the risk of Alzheimer’s. Good oral hygiene may therefore offer a simple approach to reducing the risk of acquiring the condition. Dominy urges some caution on that issue, however.
“It is very possible that P. gingivalis and the gingipains enter the brain without first causing gum disease,” Dominy points out.
Tara Spires-Jones, Deputy Director of the Centre for Discovery Brain Sciences at the University of Edinburgh, also urges caution, saying: “People with Alzheimer’s disease also have disruption of their blood brain barrier, making them more susceptible to getting infections in their brains, so while these data are interesting, it is possible that the infection is a by-product instead of a cause of disease.”
Nevertheless, Cortexyme is exploring the possibility of using drugs that inhibit the activity of the bacterial gingipain proteins to treat Alzheimer’s. They have performed preliminary tests in a mouse model of Alzheimer’s, using gingipain inhibitors that the company has designed and synthesized. The inhibitors significantly blocked amyloid protein production, reduced nerve cell inflammation and led to reduced degeneration of nerve cells.
The company has now begun a large clinical trial of one of their gingipain-inhibiting drugs. Dominy reports that they are also investigating whether P. gingivalis might also be involved in other neurodegenerative diseases.
Other avenues
Another promising avenue of recent research is also focused on bacteria, but in the gut rather than the mouth. Researchers led by Sangram Sisodia at the University of Chicago, USA, used antibiotics to alter the bacterial population of the gut in mice with a form of Alzheimer’s. They found alterations that could reduce brain inflammation and amyloid plaque formation, but intriguingly so far only in male mice3.
Researchers elsewhere are exploring the ultimate preventive measure, in the form of vaccines that could prevent Alzheimer’s ever gaining a foothold in the brain. Kiran Bhaksar and colleagues at the University of New Mexico, USA, have developed a virus-based vaccine that provokes an effective immune response against the tau proteins of Alzheimer’s, restoring some cognitive functions, but thus far only in mice4.
Research will surely push forward on many fronts to find treatment and preventive options better than the limited help that the currently available drugs can offer.
References
- Zheng, Y., Liu, A., Wang, Z-J., Cao, Q., Wang, W. et al. Inhibition of EHMT1/2 rescues synaptic and cognitive functions for Alzheimer’s disease. Brain 142, 787-807 (2019). | article
- Dominy, S. S., Lynch, C., Ermini, F., Benedyk, M., Marczyk, A. et al. Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Science Advances 5 : eaau3333 (2019). | article
- Dodiya, H.B., Kuntz, T., Shaik, S. M., Baufeld, C., Leibowitz, J. et al. Sex-specific effects of microbiome perturbations on cerebral Aβ amyloidosis and microglia phenotypes. The Journal of Experimental Medicine 216 1542-1560 (2019) | article
- Maphis, N. M., Peabody, J., Crossey, E., Jiang, S., Ahmad, F. A. J. et al. Qß Virus-like particle-based vaccine induces robust immunity and protects against tauopathy. npj Vaccines 4 Article 26 (2019) | article