16 December 2016
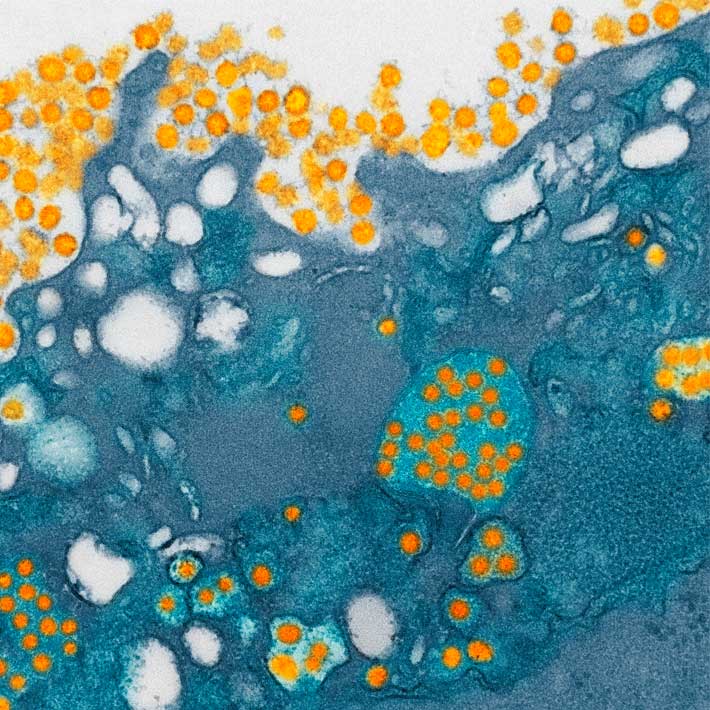
Scientists from Hong Kong have identified a blood-borne protein that signals the likelihood of hepatitis B virus (HBV) reactivation in patients undergoing high-risk immunosuppressive therapy, such as cancer patients or those with autoimmune disorders. The presence of this biomarker, called hepatitis B core-related antigen (HBcrAg), could lead to more informed decisions about when to start potentially life-saving preventive medication. This is of particular importance in the developing world, where limited resources mean judicious dispensing of medicines.
Patients undergoing acute hepatitis B infection can be diagnosed via the presence of viral surface proteins (HBsAg) in the blood. However some patients with chronic infection show no symptoms while remaining at-risk of viral reactivation. Man-Fung Yuen of the University of Hong Kong stresses that doctors need guidance on when to administer prophylaxis to these patients.
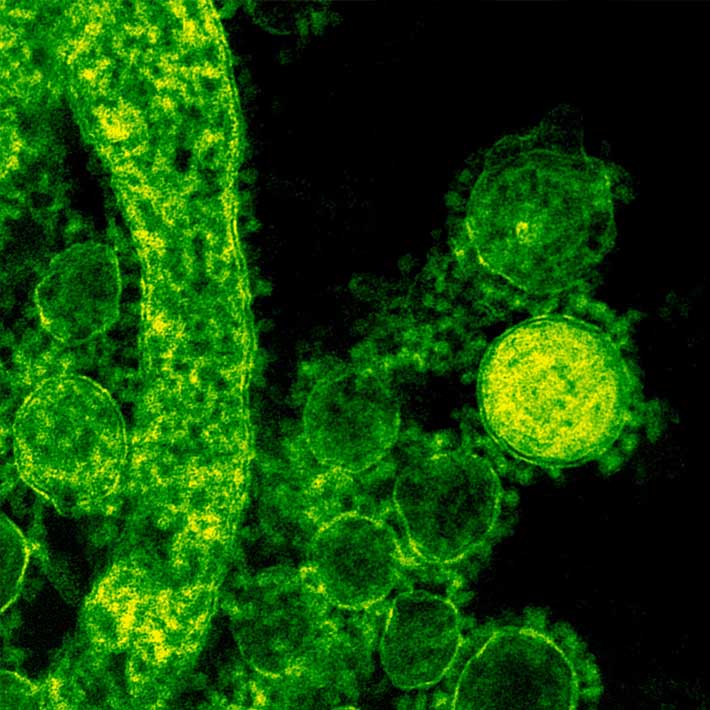
Yuen’s team studied a cohort of 124 suitable patients undergoing one of two immunosuppressive therapies: rituximab-containing chemotherapy or allogeneic (received from a genetically similar donor) hematopoietic stem cell transplantation. The patients in the study were all HBsAg-negative, but tested positive for anti-HBc (hepatitis B core) antibodies, signifying previous exposure to the hepatitis B virus. The therapies were chosen for their potent immunosuppressive effects and therefore their heightened risk of inducing HBV reactivation.
Testing for anti-HBc only indicates an individual has previously been exposed to HBV, but does not differentiate between those with a past infection from asymptomatic, chronically infected patients at-risk of hepatitis B virus reactivation.
The study group were monitored for HBV reactivation whilst levels of the biomarker HBcrAg were monitored. The team found that HBcrAg-positive patients had a much higher rate of viral reactivation, with 72% experiencing virus reactivation within two years. “HBV reactivation is becoming a common problem because of advances in using more potent immunosuppressives,” says Yuen.
In some parts of the world such as East Asia, incidence of anti-HBc-positive individuals can reach 68%, while treatments involving immunosuppressive therapy are on the rise. Where cost-effectiveness of treatment is key, Yuen hopes his team’s research will benefit patients “[by increasing] the early detection of HBV reactivation, allowing for better control of the virus before it is too late in the disease course,” ultimately improving survival rates and clinical outcomes for at-risk patients with dormant hepatitis B virus infection.
References
Seto, W., Wong, D., Chan, T., Hwang, Y., Fung, J. et al. Association of hepatitis B core-related antigen with hepatitis B virus reactivation in occult viral carriers undergoing high-risk immunosuppressive therapy. The American Journal of Gastroenterology. (2016).| article