13 October 2019
Conventional wisdom on the potential of stem cells is about treatments that directly replace unhealthy tissues — but new research suggests certain stem cells can actually wage a war against cancer cells. A team led by Mohamed Abumaree at KAIMRC has demonstrated that mesenchymal stem cells (MSCs) may have the capacity to marshal a potent antitumor immune response1.
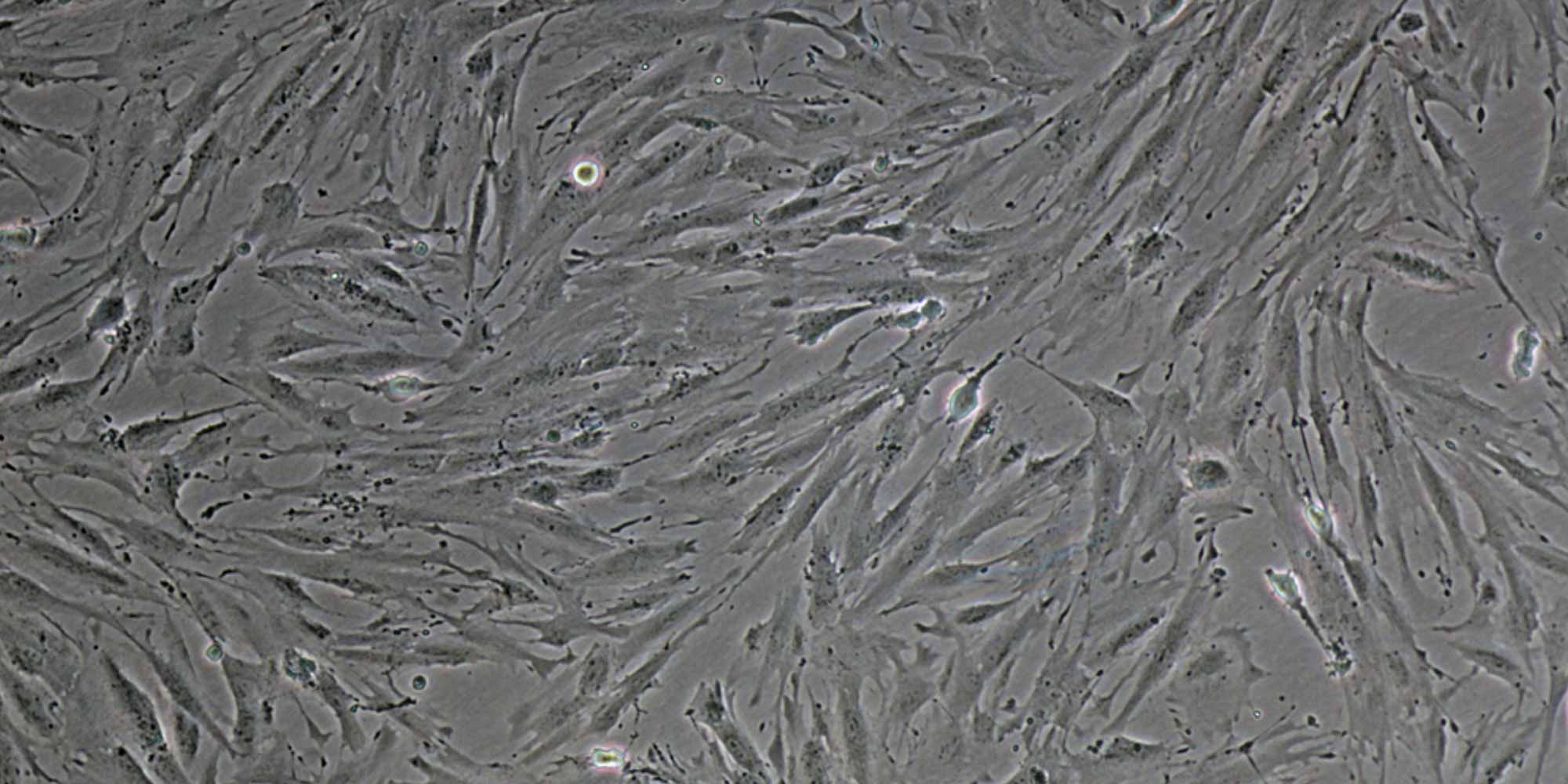
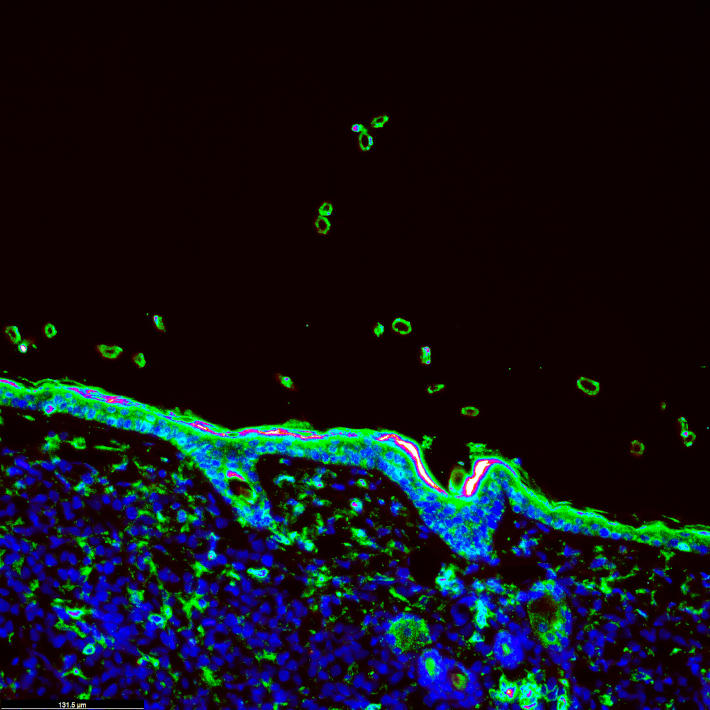
MSCs are derived from certain connective tissues in the body. These adult stem cells can form bone, fat and cartilage, but are also known to release a host of powerful biological signals that may prove valuable in treating diseases. In a paper published in Stem Cell Research & Therapy, Abumaree and colleagues identified a new subpopulation of MSCs in a section of the human placenta known as the decidua parietalis (DP), and he was intrigued by their potential clinical use.
“We found that these DPMSCs produce factors that are known to modulate the functional activities of immune cells, and to induce the expression of anticancer molecules by these immune cells,” explains Abumaree.
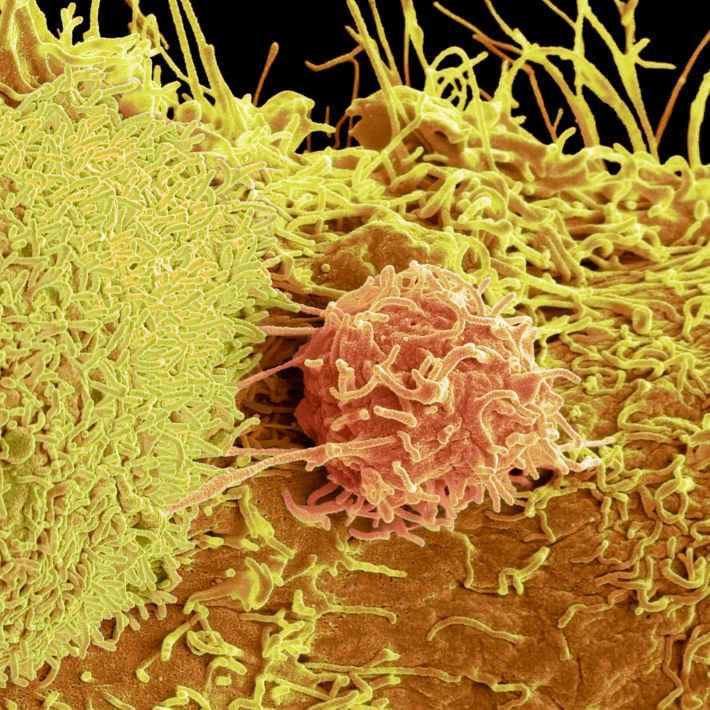
In order to evaluate the physiological effects of these signals, his team assessed the way selected subpopulations of human immune cells respond when cultured in the presence of DPMSCs. They focused on natural killer cells, which play a pivotal role in defending against tumours and viral infections, and also coordinate the broader immune response. When these natural killer cells were already biochemically activated, they attacked and destroyed the DPMSCs. But when these cells were inactivated, the DPMSCs promoted natural killer proliferation and helped switch them on by acting on a signaling protein called interleukin-18 receptor (IL-18R).
When these stem-cell-activated natural killers were transferred into cancer cell cultures, they swiftly moved to attack and destroy the diseased cells. “These DPMSCs enhance the anticancer activity of natural killer cells via mechanisms that may involve IL-18R,” says Abumaree.
However, these same immunity-stimulating properties would most likely make these cells a poor choice for the treatment of autoimmune disorders such as multiple sclerosis — an indication for which other MSC subtypes are now being tested in the clinic.
Immunotherapy has proven a powerful weapon against intransigent cancers, but it can be a challenge to rouse an effective immune response. Abumaree is therefore looking to explore whether these stem cells might be used to ‘coach’ freshly-harvested immune cells to attack tumours more aggressively. “We’re looking to educate natural killer cells in culture with DPMSCs, and then infuse these educated cells back into cancer patients,” he adds.
References
- Abumaree, M.H. et alCharacterization of the interaction between human decidua parietalis mesenchymal stem/stromal cells and natural killer cells. Stem Cell Res. Ther. 9, 102 (2018).| article