1 November 2021
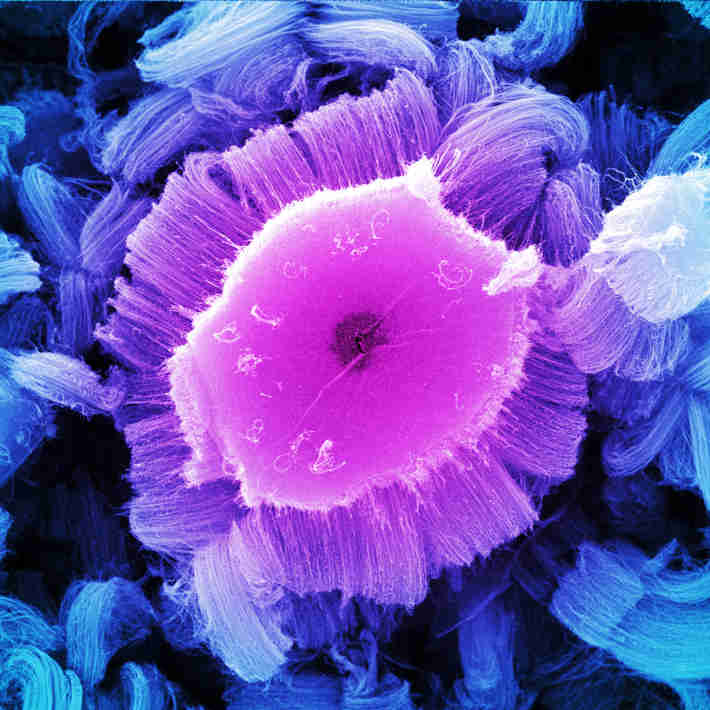
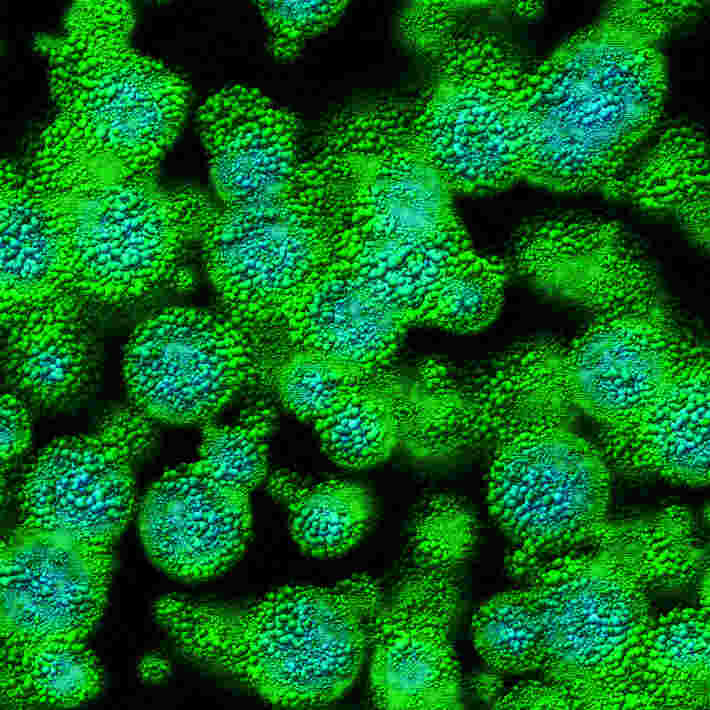
Acute lymphoblastic leukaemia (ALL) is the most common type of cancer in children. It is a white blood cell cancer that stops bone marrow from producing healthy blood cells, increasing the risk of infection.
“Thanks to recent advances in chemo- and immuno-therapies, childhood ALL has an excellent prognosis,” says Mohammed Essa, a paediatric oncologist at King Abdullah Specialist Children Hospital . Although most children with ALL are cured, around 15-20% have a high risk of relapse, and Essa explains that hematopoietic stem cell transplantation (HSCT) greatly improves survival in patients who relapse or have suboptimal response to chemotherapy.
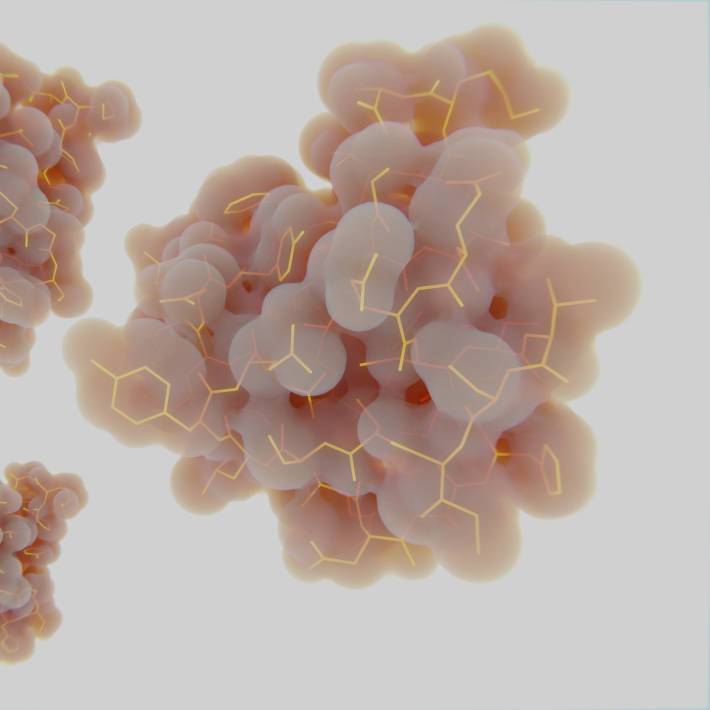
Prior to undergoing transplantation, patients receive a conditioning regimen that consists of either chemotherapy alone or chemotherapy combined with radiotherapy. The goal is to reduce the tumour burden and suppress the recipient’s immune system to allow the transplanted stem cells to make their way to the bone marrow and start making new blood cells.
Patients with ALL commonly receive total body irradiation (TBI) together with a chemotherapy drug called etoposide before undergoing HSCT. However, TBI-based conditioning can have lifelong adverse effects; it can impair growth and cognition, and increase the risk of secondary malignancies.
Essa took part in an international study led by Christina Peters at the University Vienna, Austria, which aimed to determine whether conditioning with chemotherapy (chemo-conditioning) could replace TBI in paediatric patients with high-risk ALL. The team followed the outcomes of more than 400 patients aged 18 and younger between 2013 and 2018. The patients were randomly assigned to TBI and etoposide or chemo-conditioning before HSCT. “TBI was the leader,” says Essa.
They found that patients who received TBI had a significantly lower risk of relapse and treatment-related mortality after seven years compared with patients who received chemo-conditioning. “We hoped that the outcomes would be similar with both regimens so patients could avoid the adverse effects of radiotherapy”, Essa says, “but our results confirm those of previous retrospective studies showing that TBI is better in preventing relapse”.
The authors recommend conditioning with TBI plus etoposide for patients over four-years old with high-risk ALL undergoing HSCT. However, chemo-conditioning remains an option in some cases. “Although it may not be the first-choice treatment, chemo-conditioning is still a good option when TBI is not available or contra-indicated,” Essa adds.
References
- Peters, C. et al. Total Body Irradiation or Chemotherapy Conditioning in Childhood ALL: A Multinational, Randomized, Noninferiority Phase III Study. Journal of Clinical Oncology 39, 295–307 (2021). | article