8 October 2019
Children born through in vitro fertilization (IVF) are slightly more likely to develop early childhood cancers, especially of the liver and central nervous system, according to a new study by researchers in the US. The study, conducted by the University of Minnesota, has concluded that, compared to the occurrence rate in naturally conceived children, the overall cancer rate in children from IVF may be 17 percent higher, and hepatic tumour occurrence may be 2.5 times higher.
However, the researchers emphasize that the increased risk is too small to worry people considering IVF treatment, with an occurrence rate of 252 cancer cases per million IVF births, or 0.025 percent.
In 1978, in Manchester, UK, Louise Brown was the first child born after IVF conception. The procedure accounting for 1.7 percent of US births in 2015, according to a recent survey. Livestock produced through IVF are at a higher risk of developing an overgrowth disorder, and IVF-conceived babies have greater incidence of the analogous human disorder, Beckwith-Wiedemann syndrome, which predisposes children to certain types of cancer.
“There wasn’t a huge amount of evidence saying that this should be of concern, but it was enough for us to want to investigate,” says the study’s lead author Logan Spector, a paediatric cancer epidemiologist at the University of Minnesota. Spector’s team has conducted the largest cohort study to examine the occurrence of cancer in IVF-conceived children, studying a sample that is 2.5 larger than previous studies, and publishing the results in JAMA Pediatrics journal in April 2019.
Together with researchers around the US, Spector collected data from the Society for Assisted Reproductive Technology Clinical Outcomes Reporting System (SART CORS) to find IVF births in birth registries in 14 states. They then matched these with 10 times as many non-IVF births and used the combined list to study childhood cancer rates based on data in cancer registries. They found a small association between IVF and overall cancer rates, with about 252 cancers per million IVF births, compared to 193 per million non-IVF births.
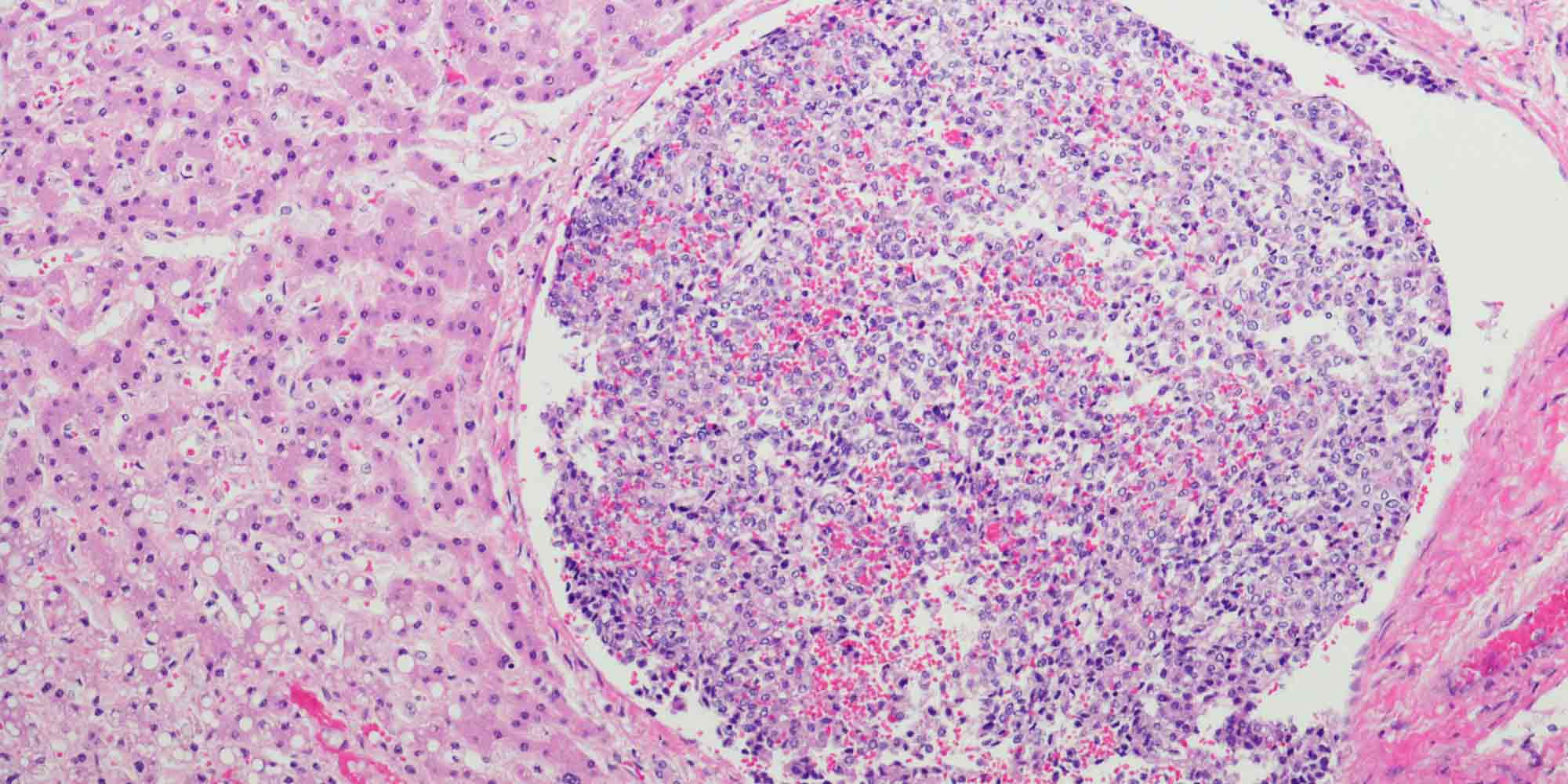
“The most important takeaway from our research is that most childhood cancers are not more frequent in children conceived by IVF,” says Spector. He explains that the slight link between IVF and overall cancer rates is largely driven by a small increase in the incidence of embryonal tumours and a doubling in the rate of liver tumours in IVF-born children. This is consistent with a 2013 UK study, which found that liver tumours were roughly three times as common among children conceived via IVF. However, the overall rate of these tumours is extremely low. Spector uses the analogy of lottery tickets to help communicate this. “A doubling in risk is scary to hear about. But if you buy two lottery tickets, even though you have twice the chance of winning, everyone would agree that your chances are still infinitesimal,” he explains.
Identifying risk factors
Marie Hargreave, a senior researcher at the Danish Cancer Society Research Center who was not involved in the study, points out that childhood cancers are very rare, especially liver tumours. She adds, however, that “childhood cancer is the leading cause of death due to disease for children in Western countries” and that even those who survive will face an increased risk of cardiovascular disease, endocrine disorders, or secondary cancers. “Identifying risk factors is important for understanding the underlying mechanisms.”
While the study measured an increase in cancer rates, the researchers were unable to determine whether this was due to the IVF treatment or underlying fertility problems which led the parents to IVF. “On a practical level it doesn’t matter,” says Spector. “If IVF enables somebody to have a child who is at a higher risk of cancer, that needs to be known wherever the risk comes from.”
However, understanding the origin of any increased risks would be the first step towards dealing with it. If the IVF process is the source of the problem, practices could be changed to reduce or eliminate risks caused by the procedure. “We didn’t identify anything that IVF clinics would have to do differently,” says Spector, commenting on the results of his current study. He has started a new project, however, to look for differences between tumours from children conceived with and without IVF. “That might help us distinguish the biological effect of IVF,” he says.
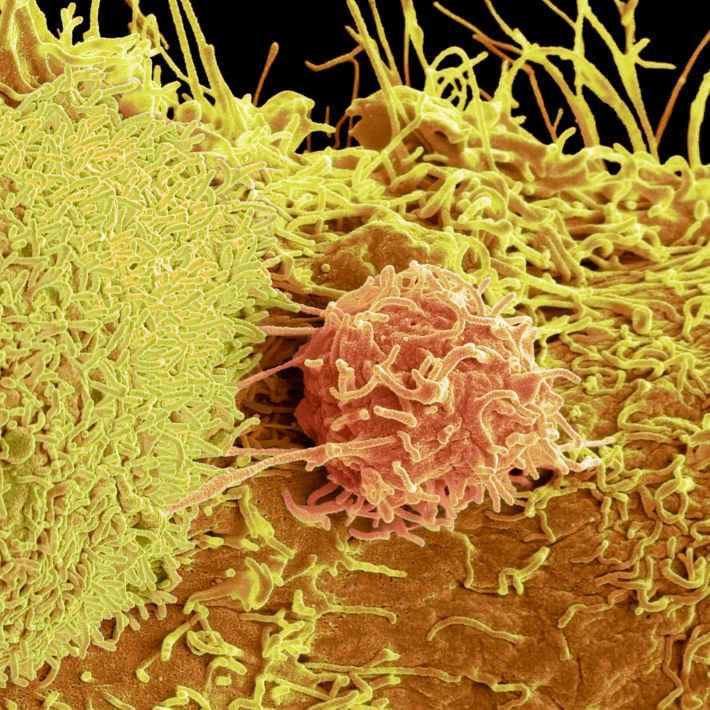
“Building on this work, DNA methylation analysis of children conceived by IVF may identify at birth those who have higher risks of developing specific cancers,” says Andrea Riccio a genetics professor at the University of Campania ‘Luigi Vanvitelli’, who was not involved in the study.
Building on knowledge
This is the latest in a series of cohort studies investigating potential links between IVF and childhood cancer, including the 2013 UK study and a 2014 study in the Nordic countries. All three studies had similar findings. Alastair Sutcliffe, a paediatrics researcher at University College London who led the UK study, calls the accumulated results “reassuring to date,” and Spector underlines the importance of carrying out parallel studies in different countries since IVF practices differ from place to place.
In addition to difference in IVF procedures, the population with ready access to IVF differs between countries, depending on whether and how it is supported by healthcare programs. In the US study, IVF was much more common among white, educated, older women, a skew which might have biased the results. “It’s a really thorny issue,” says Spector, but after further statistical analysis to test for this he says “I don’t think that it had a large impact” on the conclusions.
Hargreave adds that differences can also arise if studies include other fertility treatments alongside IVF, or even because of differences in the hormones used during fertility treatments. “This has changed over time and may be different between clinics and countries,” she says, which could affect childhood cancer risk.
The findings of all three cohort studies also overlap with the results of a meta-analysis carried out by Hargreave and others at the Danish Cancer Society Research Center in 2013, which combined data from 25 earlier studies and found a significantly increased overall risk for cancer, as well as greater risks for specific types of cancer, such as leukaemia, and central nervous system cancers.
However, the researchers interpret these results differently. For Hargreave, “the increased risk of a serious life-threatening disease in children is worrisome, aside from the other more frequent and well-established health consequences of IVF.” But Spector urges people to focus on the absolute risk, rather than the relative increase. “I don’t think that these numbers warrant a parent changing their consideration of whether they should use IVF. I would not recommend anybody change their behaviour based on this,” says Spector, adding the greater pathology during pregnancy and higher risk of birth defects associated with IVF are more likely complications for people considering the treatment.
Looking forward, Spector hopes to pool the data from this study with others in the hope that a larger data set will lead to more robust conclusions and enable further research. “It’s going to be a lot easier to pool existing studies than to try creating more,” he says, explaining that assembling the data can be a long and difficult process.
The University of Minnesota study concludes by recommending continued monitoring for cancer in IVF-born children. Spector explains that this is because different cancers peak at different ages, and the study only followed IVF-born children for seven years — long enough to cover childhood cancers such as leukaemia, which nearly always occur in the first five years, but too short to catch cancers which become more likely closer to or during puberty. But although continued surveillance is warranted, Spector hopes this study will reassure paediatricians and prospective parents that the overall risk remains extremely low. “We intentionally published this in a journal where paediatricians would notice it,” he adds.
References
Spector, L.G. Brown, M.B., Wantman, E., Letterie, G.S., Toner, J.P. et al. Association of In Vitro Fertilization With Childhood Cancer in the United States. JAMA Pediatrics 173 (2019). | article