2 August 2021
The quest to slow down or reverse the mental decline triggered by age-related inflammation in the brain has been vigorously pursued. A discovery by scientists at Stanford University School of Medicine offers insights into cellular ageing and the promise of restoring cognitive functions.
Ageing is associated with excess, chronic, low-grade inflammation, a process that specialists refer to as ‘inflammaging’ and believe is involved in many diseases, from Alzheimer’s to cancer.
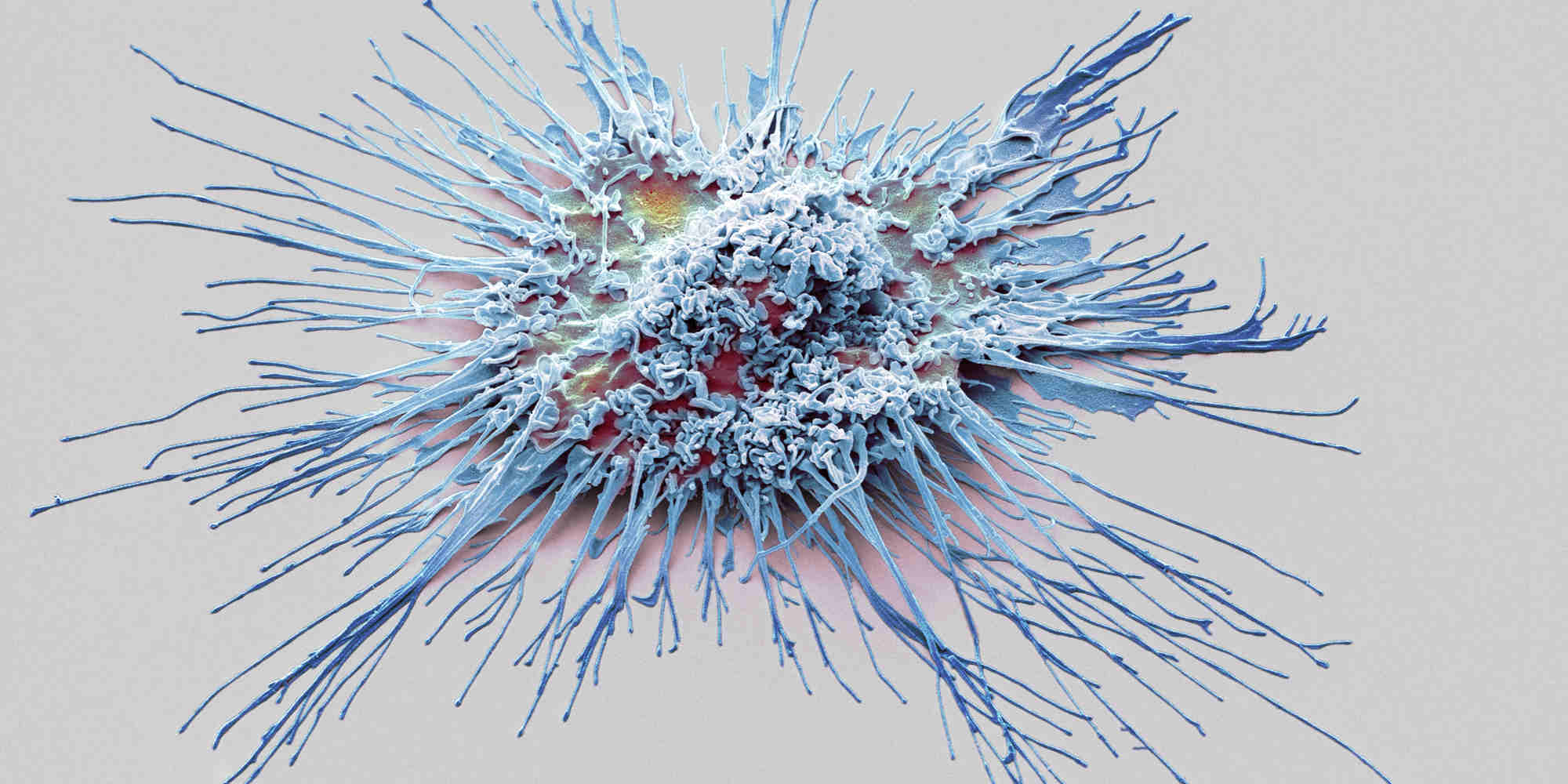
Inflammaging involves changes in the activity and biology of macrophages, specialized cells that detect and destroy bacteria and which form the first line of defence against disease-causing organisms and pathogens.
Aged macrophages store energy differently to young and healthy ones; for instance, instead of using it for fuel, they save up glycogen to use it in launching a stronger immune response during acute inflammation. But this stronger immune response, an overreaction of sorts, carries a hefty price in the aged brain; it damages normal tissue, tires the immune system, and exacerbates degenerative conditions.
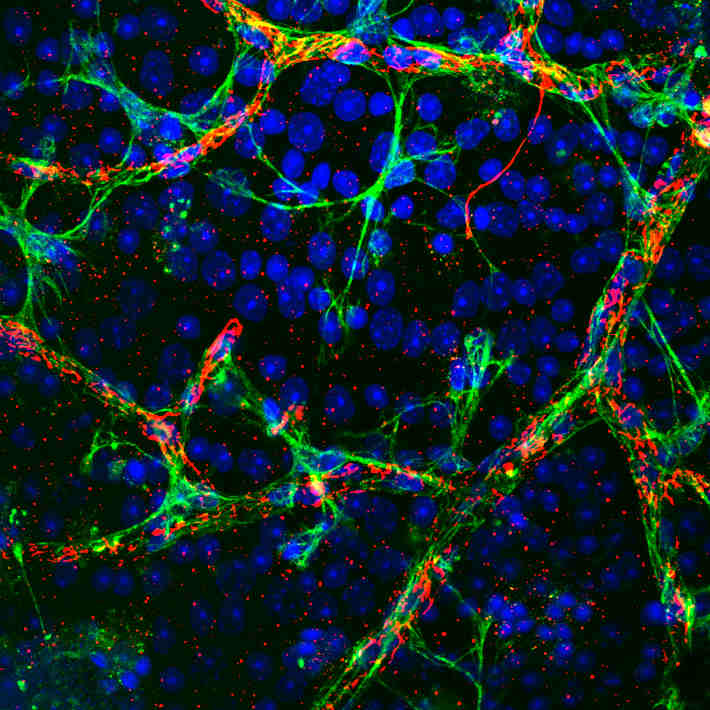
Katrin Andreasson, a professor of neurology at Stanford Medicine, is among the scientists investigating the link between metabolic activity and maladaptive inflammation. In a new study published in Nature, her team showed that microglia—the resident macrophage cells inside our brains—are highly sensitive to changes in the levels of an inflammatory molecule called prostaglandin E2 (PGE2), which they sense via the cell-surface receptor EP2.
Microglia effectively reign over the brain’s active immunity. When they are not busy battling pathogens and suppressing inflammation, they’re clearing the misfolded proteins associated with neurodegeneration1, removing old or dead neurons and cellular debris, and promoting neurogenesis by protecting and nourishing healthy and youthful neurons.
But microglia—as central as they are to brain health—can also accidently turn against the very organ they protect by going into overdrive in response to distress signals that the receptors on their surface pick up. As a result, they end up killing neurons as they try to limit infections or damage2.
Putting the brakes on cognitive decline
The team led by Andreasson used human myeloid cell cultures and aged mouse brains to investigate the links between metabolism and inflammaging in microglia. Blood-forming myeloid cells are a type of immune cell that also encompasses tissue-based macrophages.
“The levels of PGE2 increase quite significantly with ageing in both the blood and the plasma,” says Andreasson. “Obviously, we could not do a trial on thousands of human subjects, looking at different ages, but we could look at the cells. We could look at the macrophages, young and old.”
Andreasson and her colleagues found a significant difference in the level of production of PGE2 not only in young versus old macrophages, but also in young versus old serum and brain tissue.
Higher levels of PGE2 and EP2 in older microglia make them lock up their glucose as glycogen, starving them of glucose.
This problem is exacerbated by another property of aged macrophages which Andreasson and colleagues uncovered in the study. Cells can usually turn to other fuel sources for energy, such as glutamine or lactate, but Andreasson’s team discovered that aged macrophages lack that ability. They have a ‘fundamental dependence’ on glucose as a fuel source.
Together with the increased conversion of glucose into glycogen, this puts macrophages in an energy-depleted state that drives an inflammatory response.
Pinpointing a molecular pathway
The EP2 receptor came to the team’s attention in 2015 when they linked it with Alzheimer’s in a mouse model. “That got a fair bit of press,” says Andreasson. She and her team had discovered that reducing EP2 in microglia affected the Alzheimer phenotype. In fact, knocking out EP2 by 50% yielded “dramatic effects,” she says, which, together with other evidence “kind of identified this pathway as an important one in ageing.”
Treating mice with EP2 inhibitors that block PGE2 signalling reversed metabolic suppression and restored normal cell function. “The first conclusion is that you could probably reverse brain ageing by some sort of peripheral intervention,” says Andreasson. “The second is that you can reverse brain ageing by restoring youthful metabolism to your immune cells.”
By fixing the glitch in metabolism that leads to energy-deficient states in macrophages, Andreasson and her colleagues have managed to whittle down a complex cell disorder to a single molecular switch that they can toggle.
Eyal Amiel, a University of Vermont associate professor of medical laboratory science who was not involved in the study, calls this an impressive piece of work.
“What is really paradigm shifting is the simplicity of identifying a single metabolic access, a single inflammatory mediator, and a single receptor that underlie both the inflammatory and metabolic functionality of the cells, with a direct and impressive impact on neurodegeneration,” he says. “To have all of those things line up and work out is really breathtaking.”
The million-dollar question, according to both Amiel and Andreasson, is what this means in terms of mitigating or reversing neurodegenerative diseases in humans.
While human trials may still be far down the pipeline for the Stanford Medicine team, the immediate next step, says Andreasson, is to find more pathways that work in similar ways then take it from there.
“I'm not sure if there are going to be that many pathways that are going to be like this, but there might be more,” she says. “We are looking at another one right now. There might be another pathway very similar to this one that could be increasing with ageing, that suppresses myeloid metabolism, and which basically promotes these maladaptive aging inflammation responses.”
In the meantime, other approaches could help people avoid or reverse inflammaging, says Andreasson. “Keeping a healthy lifestyle, exercising, eating right—this is all associated with inflammation, and I wonder if that actually might help correct the changes in metabolism that occur with ageing,” she says. “That is something we would like to test.”