29 November 2021
Patients with diabetes are more likely to suffer serious complications from COVID-19, and scientists are trying to understand why the novel coronavirus is worse for diabetic patients and how to reduce risk.
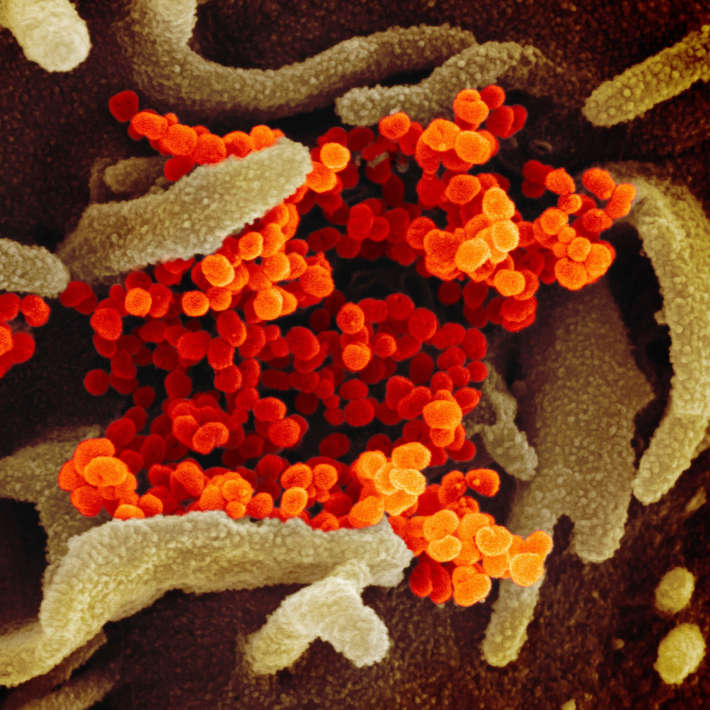
A study in Diabetes Care, authored by Justin Gregory of the Ian M. Burr division of pediatric endocrinology and diabetes at Vanderbilt University School of Medicine, Nashville, and colleagues, found that COVID-19 severity is tripled among diabetic patients¹. Elevated blood glucose enables the novel coronavirus to infiltrate cells and eventually bind to ACE2, a protein on the surface of many cells and a receptor for SARS-CoV-2. Recent studies also show that people with diabetes have chronic low-grade inflammation which contributes to the severity of illness. Other studies suggest that the number of T-cells is dramatically reduced among severe COVID-19 patients, eventually causing immune system dysfunction. Innate immune defences can also be impaired in diabetic patients.
Despite these findings, a full understanding of why diabetics have a worse prognosis remains elusive. “What I suspect is that people with diabetes, whether you’re talking about type 1, or type 2, have this condition called endothelial dysfunction, and it’s also pretty well known that people with diabetes have blood vessel disease,” says Gregory.
He explains that the blood vessels of people with diabetes are more prone to inflammation, from those that supply the backs of the eyes, retina, kidneys, or nerves to the large vessels that lead to the coronary artery. “Take someone who already has a propensity for blood vessel disease and then you stack COVID-19 on top, and it doesn’t take much to have those clots that are so problematic or for those capillaries to become leaky, and let fluid into the lungs.”
According to Gregory, there’s enough evidence to suggest that COVID-19 gets into a cell through ACE2, which endothelial cells typically highly express. “This is a key point at which SARS-CoV-2 is attacking the cell, and so I think the key vulnerability for people who have diabetes is the lining of those blood vessels.” Gregory is investigating the increase in endothelial dysfunction in diabetes patients immediately after they contract COVID-19.
So far, it’s unclear if there’s a major difference in risk between type 1 or type 2 diabetes, but the data suggests that both types are hit in similar ways. “It really depends on how you analyse the data. That was one of the driving forces behind our research,” says Gregory. “What we found is that both type 1 and type 2 diabetes patients have about a three- or four-fold higher risk of severe COVID-19 compared to people who don’t have diabetes at all.”
In their assessment, Gregory and his colleagues also adjusted for other risk factors. “If you walk into an ICU in a city with a lot of COVID-19 cases, you might think most of the people who really are sick with COVID-19 have Type 2. It’s not because people with Type 1 are at less risk. It’s because there’s fewer of them and because they are often younger as a group.”
Metformin: old drug, new insights
New studies are revealing that diabetic patients who take metformin, the first-line medication for the treatment of type 2 diabetes, show better prognosis when infected with COVID-19.
“Metformin was used in the early 20th century to treat influenza,” says Abdallah Al-Salameh of the department of endocrinology, diabetes mellitus and nutrition at Amiens University Hospital in France who led a study on metformin published in Diabetes Metab. Al-Salameh explains that metformin has some antimicrobial, anti-inflammatory, immunosuppressive, and antifibrotic properties². “All of these issues are important in COVID-19 because it is a microbial disease with a cytokine storm,”
While metformin users fare better post-infection, it’s still too early to extrapolate beyond a correlation between metformin use and the alleviation of some severe COVID-19 symptoms. It is also unlikely that giving metformin to patients who hadn’t taken the drug before hospitalization would have confer any benefits or result in noticeable improvement.
“What we know is that metformin is useful in people with diabetes to improve the severity of COVID-19, but if we give a patient metformin in the acute phase of a COVID-19, will it be useful? We need a controlled randomized study to answer this question. All we have so far are observational studies.” Al-Salameh adds that there’s no evidence to suggest that metformin can prevent infection.
Scientists are also trying to establish whether there is a link between COVID-19 and metabolic glucose disturbances. An international group of diabetes researchers created CoviDIAB, a global registry of patients with COVID-19-related diabetes, which at a later stage will incorporate pre-existing diabetics who present with severe acute metabolic disturbance. Through the registry, the researchers plan to explore the extent and phenotype of new-onset diabetes to investigate the “pathogenesis of COVID-19-related diabetes and to gain clues regarding appropriate care for patients during and after the course of COVID-19,” according to a letter published in the New England Journal of Medicine³.
Despite all the questions about the strong relationship between high blood glucose and COVID-19, Gregory points out that one tool that seems to work to pre-emptively lower the risk of infection is vaccines. “Despite the fact that people with diabetes have a higher risk of getting severe illness, the vaccine is just as efficacious for people with diabetes,” he says.
References
- Gregory J.M., et al. COVID-19 Severity Is Tripled in the Diabetes Community: A Prospective Analysis of the Pandemic's Impact in Type 1 and Type 2 Diabetes. Diabetes Care. 44(2):526-532 (2021) | article
- Lalau J.D., Al-Salameh A., et al. Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19. Diabetes Metab. 10;47(5):101216. (2020) | article
- Correspondence: New-Onset Diabetes in Covid-19, NEJM (2020) | article