1 October 2017
Transfusions to prevent bleeding after chemotherapy — in patients with blood malignancies, like leukaemia, and those undergoing haematopoietic stem cell transplantation — are more often successful in Saudi Arabia than elsewhere, according to a recent study.
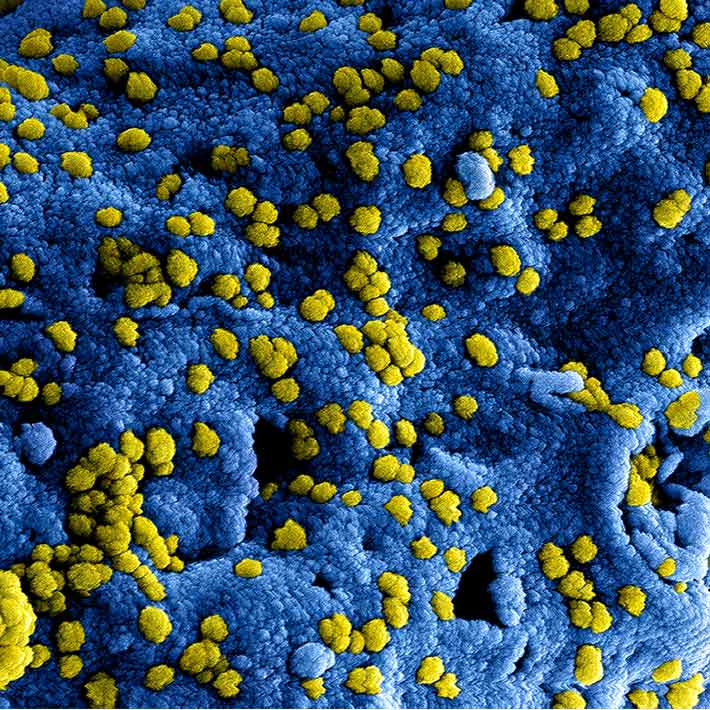
Chemotherapy decreases the platelets in a patient’s blood, reducing its ability to clot and thus increasing the risk of serious complications due to bleeding. Patients with low platelet counts are given transfusions to mitigate this risk, but these sometimes fail to increase the number of platelets, a condition known as platelet transfusion refractoriness (PTR).
While PTR rates have been measured in several populations, they haven’t been studied in Middle Eastern populations. A team of researchers tracked 29 patients at Saudi Arabia’s Ministry of National Guard Health Affairs (MNG-HA) hospital, monitoring their platelet count before and after platelet transfusions.
Four of the patients had low platelet counts after two consecutive transfusions and were diagnosed with PTR; a 14% incidence rate. Patients with acute myeloid leukaemia or non-Hodgkin’s lymphoma were more likely to develop PTR. The rate was slightly higher (17%) when measured as a fraction of the number of transfusions (102), rather than patients, but was still notably lower than the 25-35% reported in studies of other populations.
Despite the low incidence in Saudi patients, PTR should still be considered a serious problem, says King Abdullah Medical City (KAMC) oncologist Khadega Abuelgasim, who led the study. “That particular patient will be at risk of fatal bleeding complications. PTR also drains blood products from the blood bank, straining the system,” she explains.
The researchers suggest that the low rate may be due to low genetic diversity in the Saudi population, where marriages between cousins are very common. “Because of this, there’s a very high chance of having a matched donor in the Saudi population by chance,” says Abuelgasim, which improves the chances of transfusion success.
Another factor contributing to the lower incidence rate may be the way the platelets are prepared. All of KAMC’s blood products are filtered to remove white blood cells, reducing the chance of a platelet transfusion being rejected. Blood products given to chemotherapy patients are also irradiated.
The researchers recommend these measures become standard practice throughout the kingdom, though some facilities don’t have the capacity to irradiate blood products. They also highlight the need for larger, multicentre follow-up studies to measure how PTR correlates with clinical and demographic factors.
References
Abuelgasim, K., AlHumaid, S., AlOtaibi, A., AlKhashan, M., and Ali, Y. Platelet transfusion refractoriness among patients with hematological malignancies in a tertiary center in Saudi Arabia. Journal of Oncology Translational Research 2, 112-115 (2016).| article