6 February 2019
Patients with autoimmune diabetes, also known as type I, have a far narrower range of treatment options than those with the more common type II form. By combining two parallel treatments, Qinghua Wang, of the University of Toronto, and colleagues have now identified a regimen with the potential to bolster insulin production in these patients.
In type I diabetes, the ability to regulate blood glucose is destroyed as the immune system attacks and kills insulin-producing beta cells in the pancreas. Treatment involves dependence on carefully regulated, self-administered insulin doses to stay healthy. In previous work, Wang’s team learned that a neurotransmitter known as γ-aminobutyric acid (GABA) can help preserve beta cell function in mice engineered to have type I diabetes. They next wanted to bolster this effect by pairing GABA with another anti-diabetic drug. They focused on a class of agents in current clinical use that stimulate the effects of hormones known as incretins, which regulate blood sugar levels by stimulating insulin release. These drugs have proven effective in type II diabetes, which is primarily a metabolic disorder, but offer little benefit on their own in type I.
However, the combination of GABA and the incretin-boosting drug sitagliptin proved surprisingly effective. Wang and colleagues simulated type I diabetes by using a toxic compound that selectively eradicates pancreatic, insulin-producing beta cells in mice. Treatment with the two agents had an additive effect in these subjects in terms of sustaining insulin production and maintaining reasonable levels of circulating glucose.
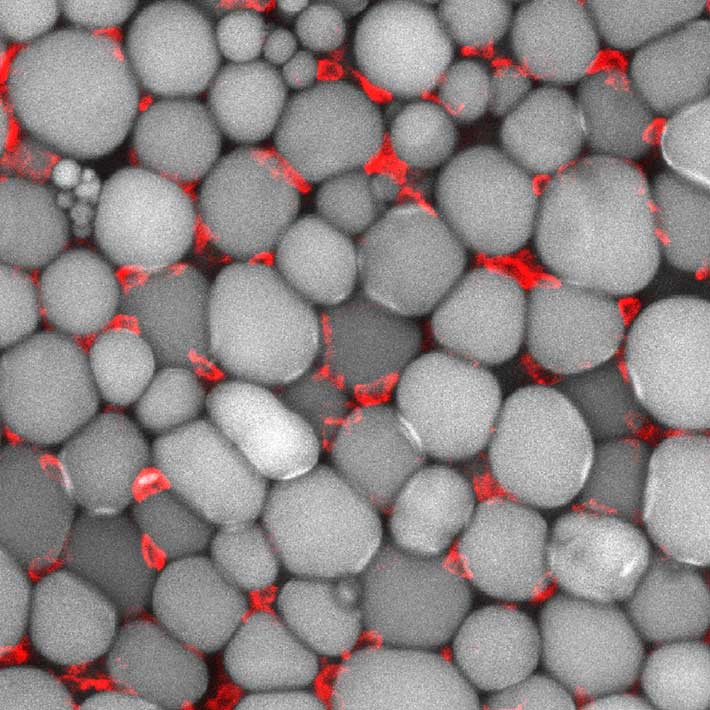
More strikingly, the researchers observed a clear rebound in beta cell populations. Either drug alone contributed to the preservation of some beta cells, but in combination the effect was doubled. Closer investigation of these cells revealed that the sitagliptin-GABA treatment simultaneously enhanced cell division while also turning off pathways that lead to cell death.
Wang and colleagues note that previous studies have suggested intriguing parallel mechanisms for these two agents. Whereas incretins have previously been linked to beta cell proliferation, GABA can potentially induce the direct conversion of pancreatic alpha cells — which contribute to elevated blood sugar — into beta cells. Importantly, both drugs can be administered orally, making them a potentially appealing therapeutic combination. “Further pre-clinical and clinical trials are warranted to test the efficacy and toxicity of combined use of GABA and sitagliptin in type I diabetes mouse models and type I diabetes human subjects,” the researchers conclude.
References
- Liu, W., Son, D.O., Lau, H.K., Zhou, Y., Prud’homme, G.J., Jin, T. & Wang, Q. Combined oral administration of GABA and DPP-4 inhibitor prevents beta cell damage and promotes beta cell regeneration in mice. Front. Pharmacol. 8, 362 (2017). | article