10 February 2019
A safe, effective method for collecting stem cells from the blood of volunteer donors has been successfully trialled by scientists at KAIMRC and clinicians at King Abdulaziz Medical City in Riyadh (KAMC-R).
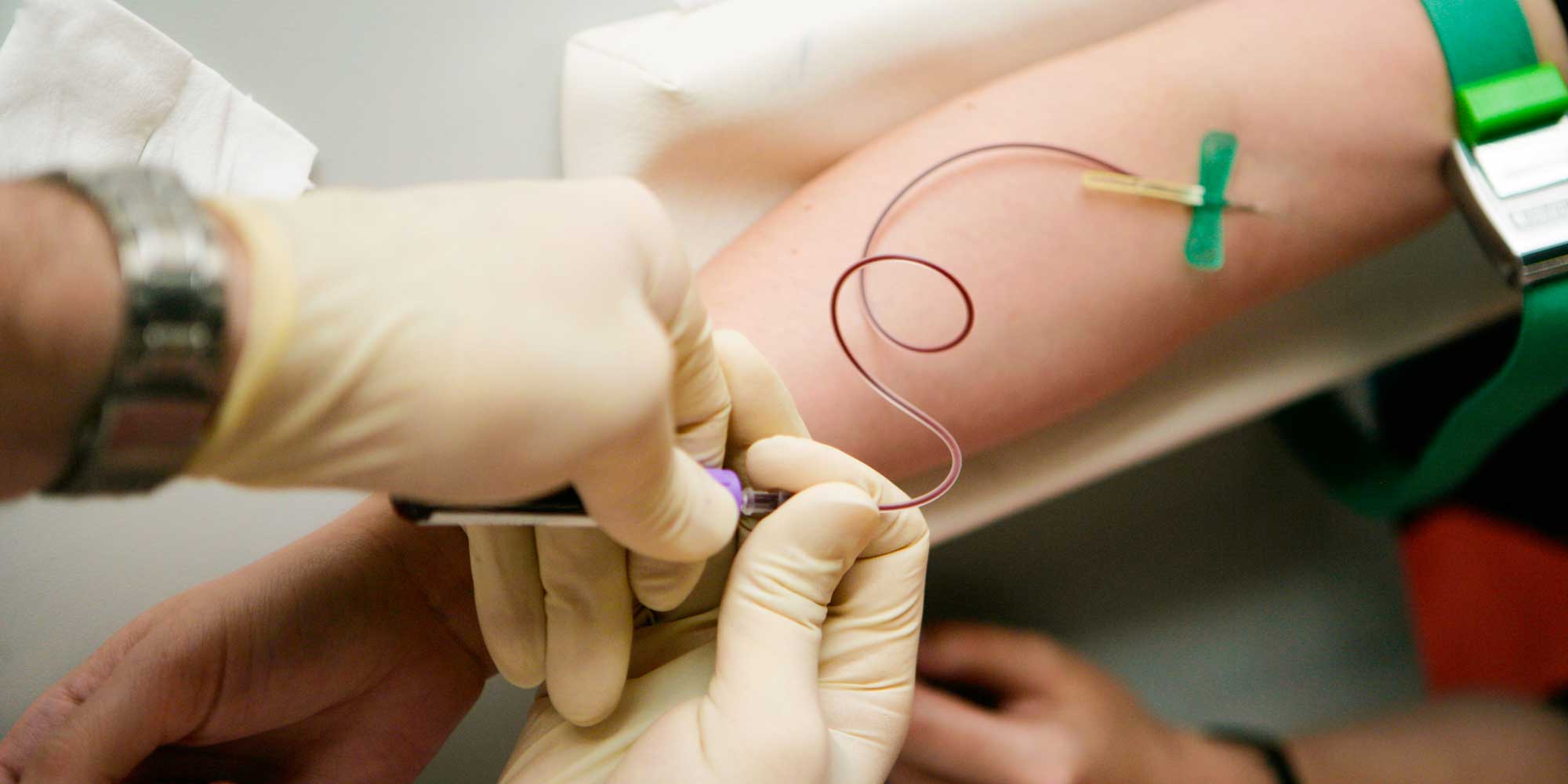
Donated stem cells provide a supply for patients with cancer, damaged bone marrow, or impaired immunity and help them generate new blood. Until recently, this process of ‘hematopoietic stem cell transplantation’ involved the use of a central line, or central venous catheter (CVC), placed into a major vein, often in the donor’s chest or thigh. A CVC was thought to be preferable because the blood needs to flow at high pressure through a filtering machine, which separates stem cells and then returns the blood to the donor’s body. Now, it is believed that the less invasive peripheral venous catheter (PVC), which taps into peripheral veins in the upper arm, is safer and may be just as effective.
“The use of CVC is still common in some hospitals in the Middle East, regardless of the donor’s ability to provide enough blood from their peripheral veins,” says Samer Ghazi at KAMC-R, who led the project. “However, inserting a CVC carries a high risk of bleeding, infection, clotting, and even death. We wanted to prove that PVCs could potentially do the job just as well in most cases.”
Ghazi’s team believes that the donation process should be guided by collaborations between different medical professionals; for example, anaesthetists, intravenous therapy specialists and haematologists. The researchers aimed to reduce CVC use at KAMC hospital to less than 20% by encouraging nurses and clinicians to work together and try to use PVCs on every adult donor.
The study, conducted over 16 months and including 42 adult donors, reduced CVC use from 72% to 0%. On the first cycle of the trial, one in four cases had to revert to CVC; this reduced to one in eight by the second cycle, and all 30 donors in the third cycle successfully provided enough blood and stem cells using PVCs without any complications.
“The advantages of switching to PVC are multiple, not least because of safety and quality of care,” says Ghazi. “PVC is readily accessible and there is no need to admit donors to the hospital, saving US00-4000 per case. It also frees up inpatient services and the radiology department, which were previously used for CVC insertion. Hopefully, our study will encourage the wider use of PVCs for stem cell donation.”
References
- Ghazi, S., Alaskar, A., Alzahrani, M., Damlaj, M., Abeulgasim, K.A. et al. Reducing central venous catheter use in peripheral blood stem cell donation: Quality improvement report. BMJ Quality Improvement 6, u211975.w4817 (2017). | article