10 February 2019
LA review of data from 20 independent studies suggests that saliva-stimulating drugs are better than other options for managing the effects of radiotherapy-induced salivary gland damage.
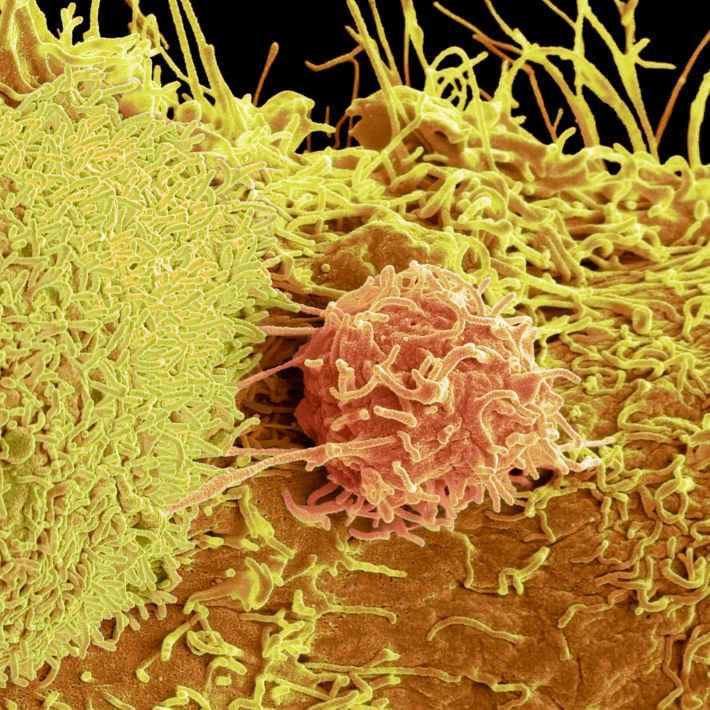
Head and neck cancers can be successfully treated with radiotherapy, however it can cause irreversible damage in up to 93% of patients if the salivary glands are within the irradiated field.
Salivary gland damage reduces secretion, which in turn can cause the unpleasant sensation of dry mouth, oral infections, dental disease, altered taste, as well as difficulties speaking and eating. Despite the high incidence of this radiotherapy-associated adverse effect, clinicians have no clear evidence-based guidelines to inform the management of reduced salivary gland function.
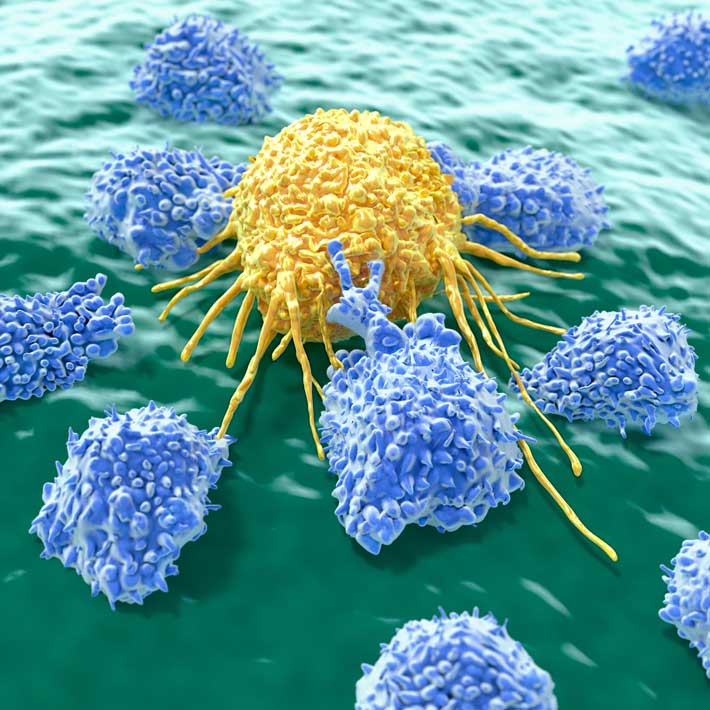
Arwa Al Hamad, at King Abdulaziz Medical City in Riyadh, and colleagues in the UK conducted an extensive review of data from 20 independent studies to determine the effectiveness of acupuncture, low-level laser therapy, herbal remedies, salivary substitutes and drugs that stimulate saliva production in a total of 1,732 patients with head and neck cancer.
Evidence supporting the use of salivary substitutes or mouth care systems that help moisten oral tissues and lessen discomfort caused by dry mouth was very weak. “Our results were surprising as these products are usually considered the first line of treatment in the clinic,” she says.
Only long-term administration of pilocarpine and cevimeline, two drugs that stimulate the glands to produce more saliva, significantly relieved dry mouth. Both compounds activate cell receptors that promote fluid secretion. Cevimeline specifically targets receptors found on tear and salivary glands. Thus, it produces fewer side-effects than pilocarpine, which stimulates secretory cells throughout the body including sweat glands, causing excessive sweating in patients.
The duration of increased salivary flow after taking the drugs is unclear. Although patients reported feeling better after taking them, the available data suggests their efficacy was short-lived.
“These results have important practical implications as clinicians managing patients with post-radiotherapy salivary gland damage should consider prescribing long-term cevimeline or pilocarpine therapy to ameliorate some of the symptoms even if the improvements are likely to have a short duration,” explains Al Hamad.
A new oral medicine clinic established at King Abdulaziz Medical City will enable further investigation into the treatment of salivary gland damage and other oral lesions.
References
- Mercadante, V., Al Hamad, A., Lodi, G., Porter, S. & Fedele, S. Interventions for the management of radiotherapy-induced xerostomia and hyposalivation: A systematic review and meta-analysis. Oral Oncol. 66, 64-74 (2017). | article