24 September 2019
In 2017, one Middle East respiratory syndrome (MERS) patient in Riyadh was responsible for directly infecting 16 patients, leading to an outbreak that infected 44 people in the surrounding area in just over a fortnight. Recent research into the outbreak indicates that it is often difficult to diagnose pneumonia, one of the key symptoms of the disease, in patients suffering renal and cardiac failures. This delays identification of the virus, and proper infection control procedures.
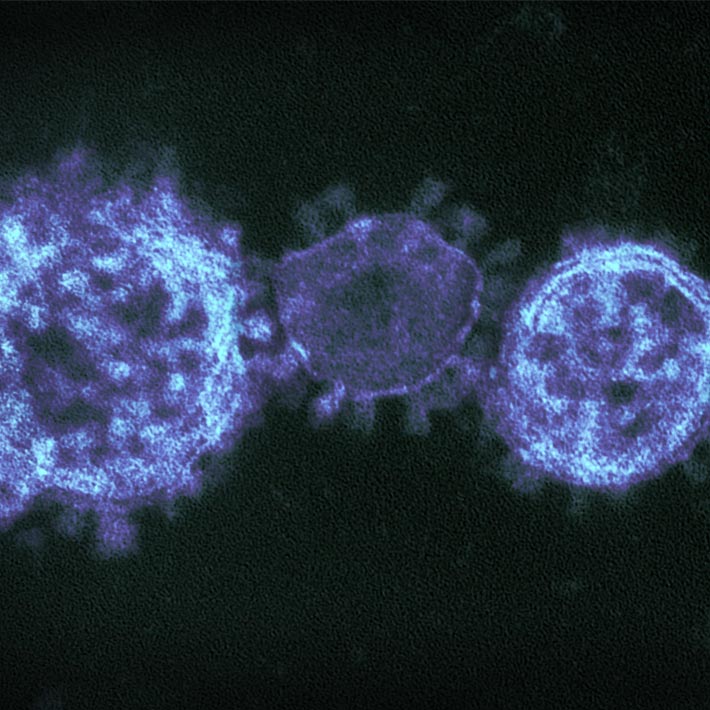
The Middle East respiratory syndrome (MERS) is a viral illness included in the World Health Organization’s priority list of diseases that need to be closely watched due to their potential to cause an epidemic. Caused by a type of coronavirus, MERS-CoV, was first identified in 2012, and is transmitted through contact with infected camels or people. There is no known cure and 35 percent of the reported patients have died. There have been at least 845 MERS-CoV-related deaths in 27 countries since September 2012. Approximately 80 percent of the reported cases are from Saudi Arabia.
Learning from past outbreaks is essential to improve infection control. A team of researchers, from universities and researcher centres affiliated with the Saudi Ministry of Health, and the Ministry of National Guard Health Affairs, have now examined the factors that led to an outbreak in Riyadh in 2017. Between 31 May and 15 June of that year, 44 cases of MERS-CoV were reported at three healthcare centres. Eleven patients died from their infections.
Of the total number of people infected, 29 were from King Saud Medical City (KSMC), the largest hospital in Saudi Arabia.
Focusing on those affected at KSMC, the researchers describe how a single patient became a ‘superspreader’ — an individual who infects a much greater number of people than average.
The outbreak was traced to a 46-year-old Yemeni man who, after arriving at the hospital by ambulance, spent 14 hours in the emergency department. His symptoms included coughing and shortness of breath, and the doctors noted that he had diarrhoea for the two previous days. Blood tests initially indicated that he was suffering from kidney failure.
To undergo haemodialysis (a routine process of cleansing the blood for patients whose kidneys are not functioning), he was transferred to a medical ward, where he shared a room with four other patients for two days.
His condition did not improve. He had trouble breathing and was admitted to an intensive care unit. At this point that the medical team suspected a MERS-CoV infection, and a nose and throat swab sample confirmed their suspicions.
The man was isolated and transferred to Prince Mohammed bin Abdulaziz Hospital, a referral centre for MERS patients where he died 22 days later.
By mapping the patient’s journey from the ambulance to the different sites in the hospital, the study showed he came into direct contact with 120 people: 107 health care workers and 13 patients. Nine of the 107 health care workers and seven of the 13 patients tested positive for MERS-CoV. It took 30 days for the outbreak to be brought under control.
The researchers conclude that “In MERS-CoV endemic countries, there is an urgent need for developing rapid point-of-care testing that would assist emergency department staff in triaging suspected cases of MERS-CoV to ensure timely isolation and management of their primary illness and prevent major MERS-CoV outbreaks.” They also recommend that continued training of the growing number of expatriate healthcare workers in Saudi Arabia is needed to help prevent future outbreaks.
References
- Amer, H., Alqahtani, A., Alzoman, H., Aljerian, N. and Memish, Z. Unusual presentation of Middle East respiratory syndrome coronavirus leading to a large outbreak in Riyadh during 2017. American Journal of Infection Control 46 1022–1025 (2018). | article