14 August 2016
Women may be at greater risk of dementia because they are more prone to the degeneration of proteins with integral roles in communication and energy provision for the brain.
Scientists, who have identified molecular clues to the basis of gender differences in the prevalence of dementia, hope the discovery will hasten the hunt for new treatments.
Dementia is a general term used to describe several different diseases of the brain that cause varying symptoms, including problems with memory, language and information processing. It frequently occurs with cerebrovascular disease (CVD) such as stroke.
Women are more likely than men to develop dementia, and cases among female patients are, on average, more severe.
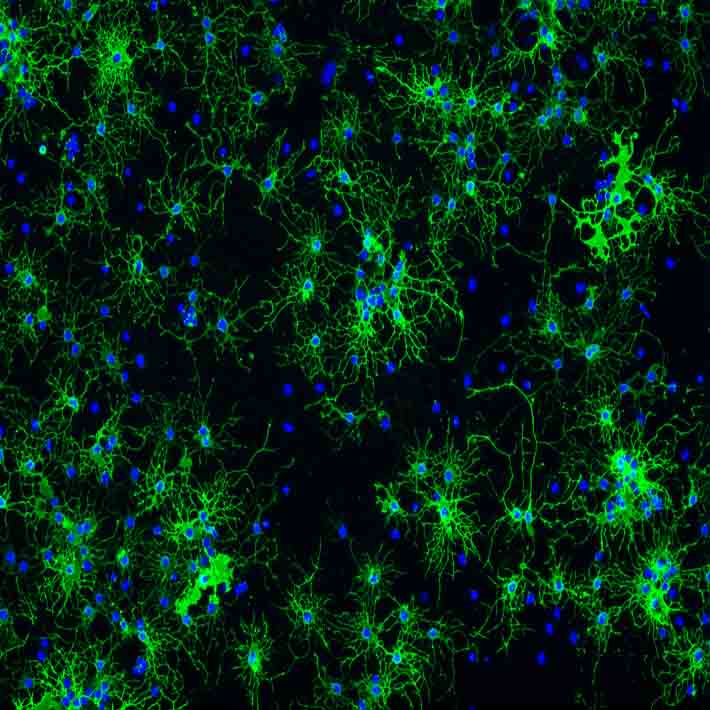
Singapore-based researchers used this gender difference to learn about the link between damage to the white matter that forms connections between brain cells and the degeneration of small blood vessels in the brains of those with dementia associated with CVD.
When they assessed brain samples from deceased patients, they initially found no differences between genders in the loss of myelin, the protective sheath that surrounds nerve cell connections.
In contrast to the more traditional analysis of one or two proteins at a time, the group, led by biological scientist Siu Kwan Sze from Nanyang Technological University, used an advanced proteomic approach to measure levels of several thousand proteins at a time.
Loss of cognitive functions in dementia patients has been found to be associated with accumulations of certain damaged proteins that have undergone spontaneous chemical reactions, called degenerative protein modifications (DPMs), which alter their structures and functions.
Using mass spectrometry, Sze found samples from dementia sufferers exhibited greater accumulations of degenerated myelin basic protein (MBP), which is important for maintaining nerve cell connections, and of other proteins associated with brain signalling.
Specifically, he found increased degenerative protein modifications called citrullination and deamidation in MBP in samples from female patients.
Sze believes that in healthy people, degenerated MBP is usually degraded by a specific set of enzymes, and that reduced production of these enzymes ultimately impairs brain signalling, and causes brain cell death and dementia.
When the researchers looked at proteins in the mitochondria, they found lower levels of a set of enzymes that synthesise adenosine triphosphate (ATP), the molecule that stores and transports energy, in the female samples.
This is consistent with previous reports of women with cognitive disorders having impaired metabolism in the brain and suggestions of mitochondrial dysfunction.
“We are the first to find these gender-specific modifications at the molecular level,” says Sze. “A better understanding of the molecular mechanisms that explain why women are more likely to get dementia could lead to the development of new diagnostic and clinical interventions.”
References
- Gallart-Palau, X., Lee, B., Adav, S., Qian, J., Sze, S. et al. Gender differences in white matter pathology and mitochondrial dysfunction in Alzheimer’s disease with cerebrovascular disease. Molecular Brain (2016). | article