14 August 2016
The heightened risk of liver cancer associated with chronic hepatitis B infection is not reduced even if the virus is cleared from the bloodstream, according to recent research. The study, which improved on previous attempts to assess the risk, demonstrates that continued monitoring for liver cancer is warranted in everyone with chronic hepatitis B infection.
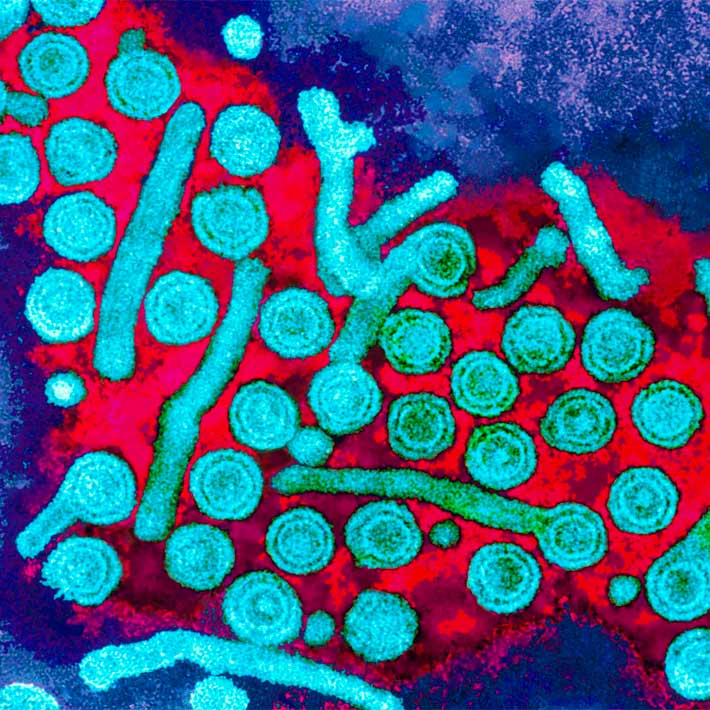
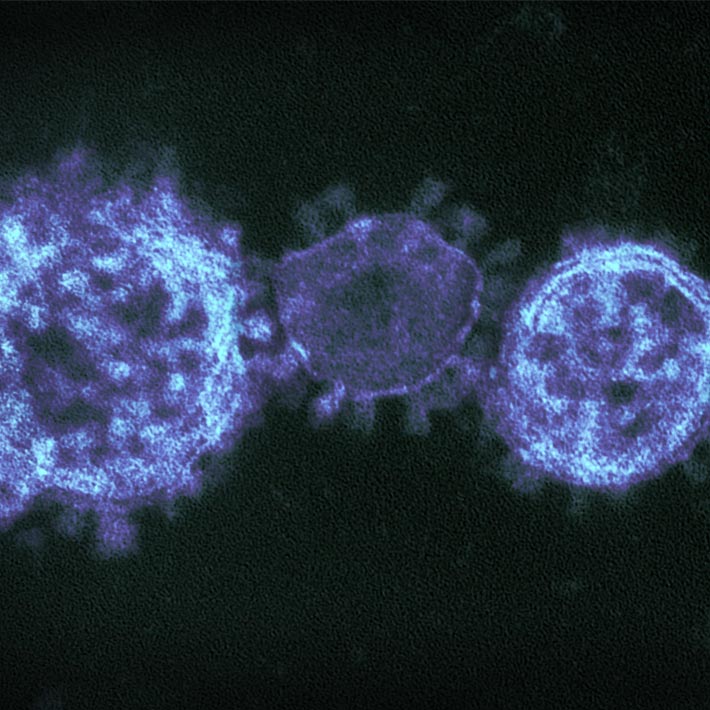
Chronic infection with the hepatitis B virus (HBV) affects 248 million people worldwide, and increases the risk of liver cancer. Chronic infection can never be cleared completely, as the DNA of HBV integrates into the human genome. However, in some patients, the active virus is cleared from the blood, detected as a negative test for hepatitis B surface antigen (HBsAg).
It has long been unclear if the subsequent risk of liver cancer is lower if the virus clears from the blood, and guidance on monitoring these patients is lacking. Prabhu Gounder, from the Centers for Disease Control and Prevention in the US, and his colleagues aimed to provide some clarity.
Gounder and co-workers analyzed data from a population of native Alaskans first followed in the 1980s as part of a statewide HBV vaccination campaign. Those with chronic HBV infection, regardless of the presence or absence of HBV in their blood, were subsequently monitored for liver cancer over a period of 30 years. Gounder and his team designed a study to give them an advantage over earlier work.
“Previous studies included the time during which individuals were HBsAg positive when evaluating the risk of liver cancer,” explains Gounder. “We hypothesized that this might have diluted [a potential] protective effect of losing HBsAg. In our study, we isolated the time period after losing HBsAg and compared that with the equivalent time period among individuals who did not lose HBsAg.”
The analysis revealed that clearance of active HBV from the blood did not reduce the subsequent risk of developing liver cancer. The result, says Gounder, is in line with the understanding that early factors in HBV infection, such as the amount of virus in the blood and the extent of liver inflammation, influence the risk.
“The key point is that individuals with chronic HBV infection have an increased lifetime risk of developing liver cancer, even after resolving chronic infection,” states Gounder. He warns that the conclusions need to be confirmed in larger populations, but in the meantime suggests clearer guidance on the basis of the new evidence: “Anyone with current or past chronic infection should be monitored closely for liver cancer.”
References
Gounder, P. P., Bulkow, L. R., Snowball, M., Negus, S., Spradling, P. R. et al. Nested case–control study: hepatocellular carcinoma risk after hepatitis B surface antigen seroclearance. Alimentary Pharmacology and Therapeutics (2016).| article