3 June 2021
An improvement in the Saudi Stem Cell Donor Registry (SSCDR) means that patients in need of stem cell transplants will have a lower risk of complications. The addition of sequence data from the immune genes of potential donors reduces the chance of a mismatch.
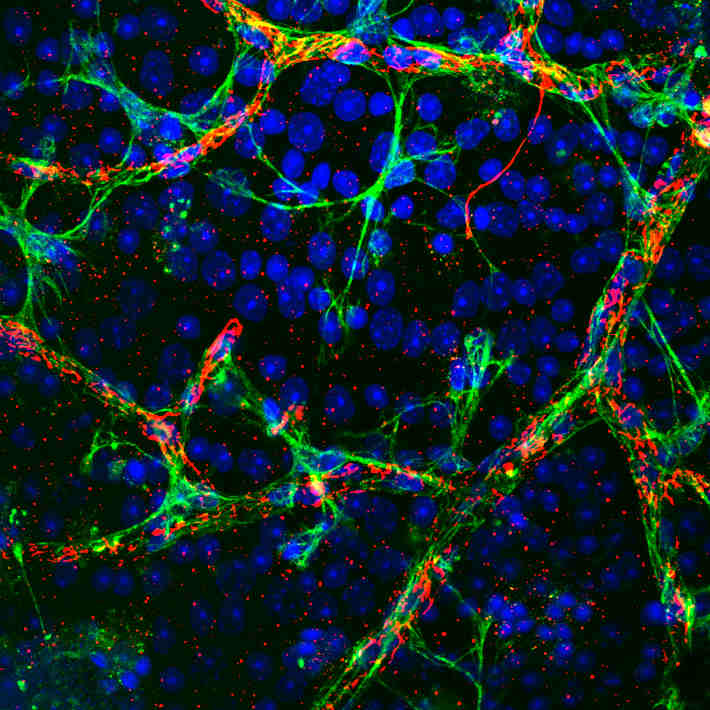
SSCDR launched in 2011 by King Abdullah International Medical Research Center(KAIMRC) and the Ministry of National Guard- Health Affairs, lists more than 75,000 registered potential donors who are willing to donate their blood-forming hematopoietic stem cells (HSCs) to patients in need worldwide with life-threatening diseases such as leukaemia. Transplanted HSCs can reboot the production of healthy blood cells, but they need to be compatible with the patients’ immune system.
Human leukocyte antigen (HLA) genes play a key role in determining the success of HSCs transplantation. HLA genes produce cell surface proteins that bind to bacteria, viruses and cancer cells, and activate the immune system to attack them. The frequency and distribution of HLA alleles differ widely between different ethnicities and geographical areas.
“Matching HLA alleles between patient and donor in stem cell transplantation is an important factor for a successful outcome,” says KAIMRC’s Ali Hajeer, founder of the SSCDR, and lead author of the new study. A mismatch between donor and recipient HLA alleles can lead to organ rejection, graft failure and cause graft versus host disease, a major post-transplant complication in which donated cells recognize the host’s cells as foreign and attack them.
The new study describes the frequencies of HLA types in nearly 29,000 Saudi stem-cell donors. “By sequencing such a large population, we found many new alleles that were not known before and were first reported in the Saudi population, and we identified new associations between different genes of the HLA system that are not seen in other populations,” Hajeer explains.
These data can be used to predict the chances of finding a compatible unrelated donor for patients who need a stem cell transplant but don’t have an HLA-compatible relative. Although the chances of finding an HLA-matched relative are quite high in Saudi Arabia due to the high rate of consanguineous marriages, it is estimated that up to 40% of patients cannot find a matched HSCs donor within their family.
The results also provide a useful starting point for investigating associations between particular HLA alleles and autoimmune diseases such as type I diabetes, rheumatoid arthritis and celiac disease, among others. “We will continue sequencing HLA and other polymorphic genes in our donors creating a larger Saudi cohort to further understand the genetic basis of the immune response in Arabs,” Hajeer says.
References
- Jawdat, D., et al. HLA-A, -B, -C, -DRB1, -DQB1, and -DPB1 Allele and Haplotype Frequencies of 28,927 Saudi Stem Cell Donors Typed by Next-Generation Sequencing. Front Immunol. 11, 544768 (2020). | article