29 April 2020
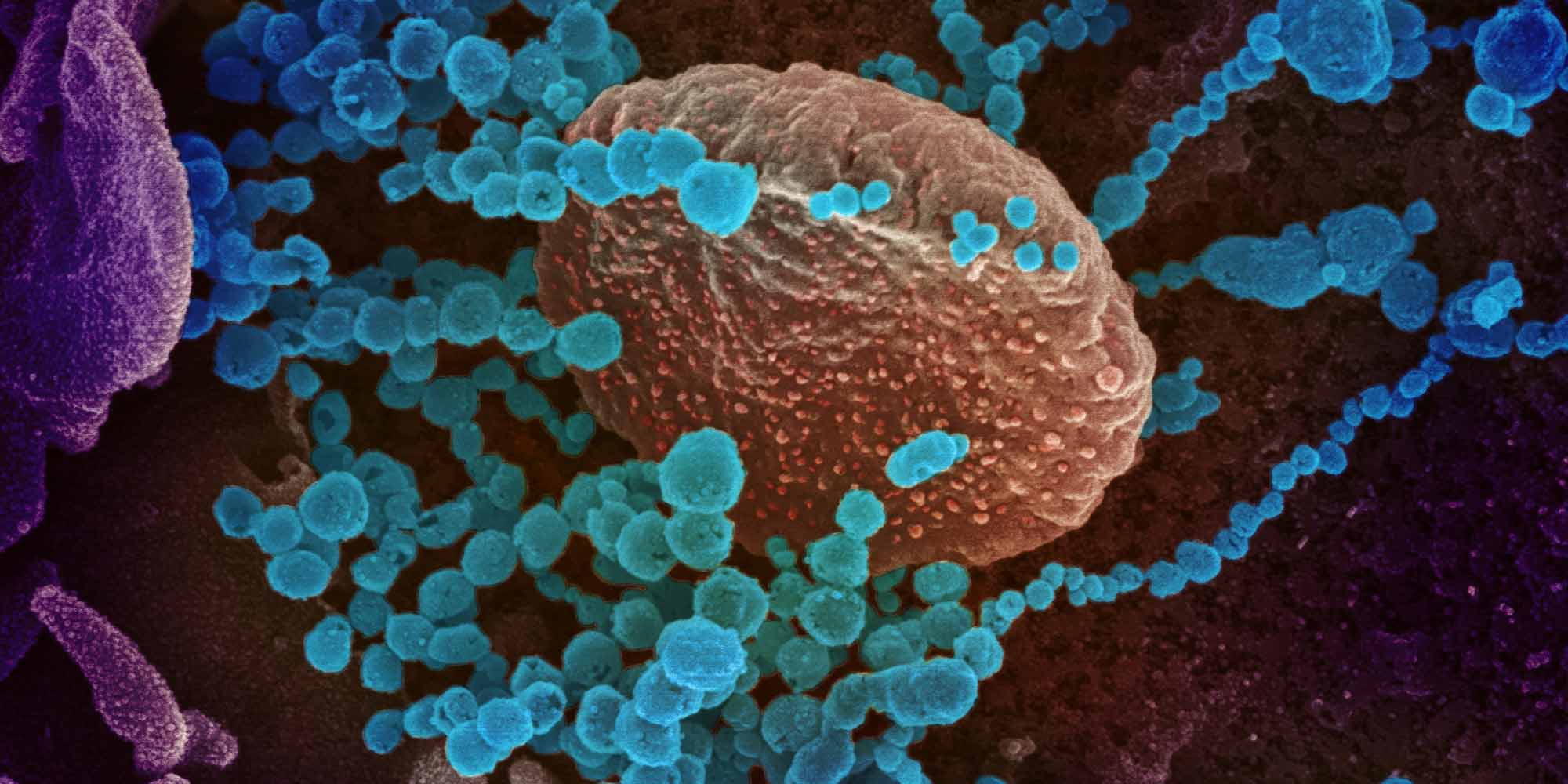
It is difficult to process the deluge of news about the coronavirus (SARS-COV-2) responsible for the COVID-19 pandemic. Scientists, clinicians and public health experts are still struggling to get a handle on this pathogen, which was completely unknown just six months ago. Myths and misconceptions can spread quickly in this environment, but there is information available to help the public to better protect themselves and their loved ones.
We are yet to understand various aspects of the SARS-COV-2. Research1 has concluded the virus stays in the air for up to three hours under the specific hospital settings because inserting breathing tubes in COVID-19 patients makes the virus spread, and stay in the air, more aggressively. Scientists, however, can still not say that the virus is airborne. Policymakers are still trying to determine whether mask use should be common advice. Some facts about the respiratory virus that affected almost 3 million around the world, however, are well established.
Myth: Only old people need to worry about COVID-19
Elderly people are at greatest risk of severe disease or death from coronavirus infection. One recent study2 in Italy found that the median age of patients admitted to the intensive care unit (ICU) was 63 years old, and mortality rates were more than twice as high for those patients over 63. However, patients as young as 14 were hospitalized, and a report3 from the US Centers for Disease Control and Prevention found that 20% of American ICU patients were between the ages of 20 and 44. And as for the many young people who remain asymptomatic after infection, they are still contagious and can spread the disease, putting older family members, neighbours, and coworkers at considerable risk.
Myth: The COVID-19 coronavirus originated in a laboratory
The larger family of coronaviruses are well-known ‘zoonotic’ agents—meaning, pathogens that can make the leap from animal hosts to humans. In the past 20 years, the world has already seen multiple outbreaks from deadly coronaviruses that originated in species such as bats or camels, including the severe acute respiratory syndrome (SARS) outbreak of 2002–3 and Middle East respiratory syndrome (MERS), which first emerged in 2012. All available evidence indicates that the SARS-CoV-2 virus responsible for COVID-19 is directly descended from a natural bat-borne virus. In a recent study4 from Nature Medicine, a team of scientists from the US, Australia and UK analyzed the SARS-CoV-2 genome, and report that “our analyses clearly show that SARS-CoV-2 is not a laboratory construct or a purposefully manipulated virus.”
Myth: COVID-19 is less dangerous than the flu
Seasonal and pandemic influenza are both major threats to health and life—Johns Hopkins estimates that flu virus infection is responsible for between 291,000 and 646,000 deaths worldwide each year. In contrast, COVID-19 has already caused upward of 200,000-plus deaths as of late April — just five months since the virus first appeared. It should also be noted that the COVID-19 death toll is in spite of social distancing, surveillance, and infection control measures taken by many countries. Furthermore, both vaccines and therapeutics are available to mitigate influenza, whereas no such protection is currently available for COVID-19, creating the potential for a much deadlier situation if strong public health measures are not maintained. COVID-19 is also more contagious than the flu; and each COVID-19 patients infects between 2.2 to 2.5 others, whereas the rate in the flu is only 1.3. Flu mortality rate is also less than 1%, whereas early estimates of the World Health Organization puts the rate for COVID-19 at 3.4%.
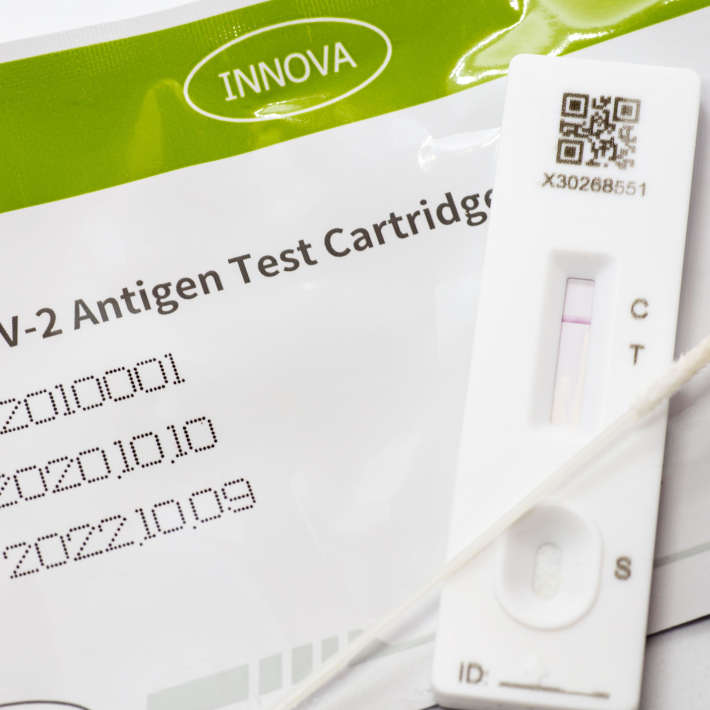
Myth: A mask is sufficient to protect against catching COVID-19
In many countries, members of the public are being encouraged or even required to wear a surgical or cloth mask when in public during the pandemic. Masks can help reduce the spread of infection and are a good precaution, but should not be seen as complete protection. A report5 published in Nature found that individuals who wear homemade cotton masks or surgical masks are less likely to spread droplets containing the virus when they breathe or talk, and can thus help protect others in the community from infection. However, wearing a mask will not necessarily prevent against contracting COVID-19 from unmasked individuals. It is essential that the mouth and nose are both fully covered, that the wearer refrains from touching either their face or the mask while in use, and that the mask is either immediately discarded afterward (for surgical masks) or washed before reuse (for fabric masks). And even with a mask, appropriate social distancing remains essential for maximum protection. It is also important to remember that the virus can also be caught through the eyes.
Myth: Pets can spread COVID-19
To date, there have been a few reports of animals testing positive for infection with the SARS-CoV-2 virus, including one cat in Belgium, and a two dogs in Hong Kong. However, there is currently no evidence to suggest that this virus can cause active disease in these animals, and likewise, there are no indications that animals carrying the virus can transmit it to humans. One laboratory study that is in preprint has demonstrated that cats can spread the virus to other cats in an experimental setting, but none of these animals developed disease, and it remains unclear whether similar spread between animals occurs in the real world. The American Veterinary Medical Association has announced that they “have no information that suggests that pets might be a source of infection for people with the coronavirus that causes COVID-19,” although they advise that patients with active infection should limit their contact to pets until they recover.
Myth: Warm spring and summer weather will slow the spread of COVID-19
In temperate climates, cold and flu season typically spans from late fall to spring. The reasons for this are not fully understood, but some experts6 believe that the airborne droplets that spread these viruses are more stable in the low-humidity winter air than in the damper summertime air. Our mucus membranes and immune systems may also be more vulnerable to infection in the winter. Although there is some evidence that COVID-19 is also somewhat hindered by warmer weather, many leading virologists see little reason to believe that summer will meaningfully hamper the pandemic’s spread, including Harvard researchers in a recent study7 published in Science. This is largely due to the novelty of the SARS-CoV-2 virus; even if weakened by heat or humidity, human immune systems are ill-equipped to fend it off, relative to familiar foes like cold or flu viruses.
References
- Doremalen,V. et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. New England Journal of Medicine. 382. (2020) | article
- Grasselli G. et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. (2020). | article
- Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep 69, 343-346 (2020). | article
- Andersen, K.G., et al. The proximal origin of SARS-CoV-2. Nat Med 26, 450–452 (2020). | article
- Leung, N.H.L., et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med (2020). | article
- Shaman, J. et al. Absolute humidity and the seasonal onset of Influenza in the Continental United States. PLoS Biol 8(2) (2010) | article
- Kissler, S. et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. | article