22 November 2021
Laboratory PCR testing for COVID-19 is highly accurate but requires specialist equipment, trained personnel, time, and infrastructure to produce and report results. In recent months, ‘antigen point-of-care tests,’ or AgPOCTs, have hit the European market with the promise of offering fast, cheap, accessible testing. A research collaboration from Germany tested a selection of these new devices and found that they have the potential to inform novel public health decisions and provide a new tool for clinicians.
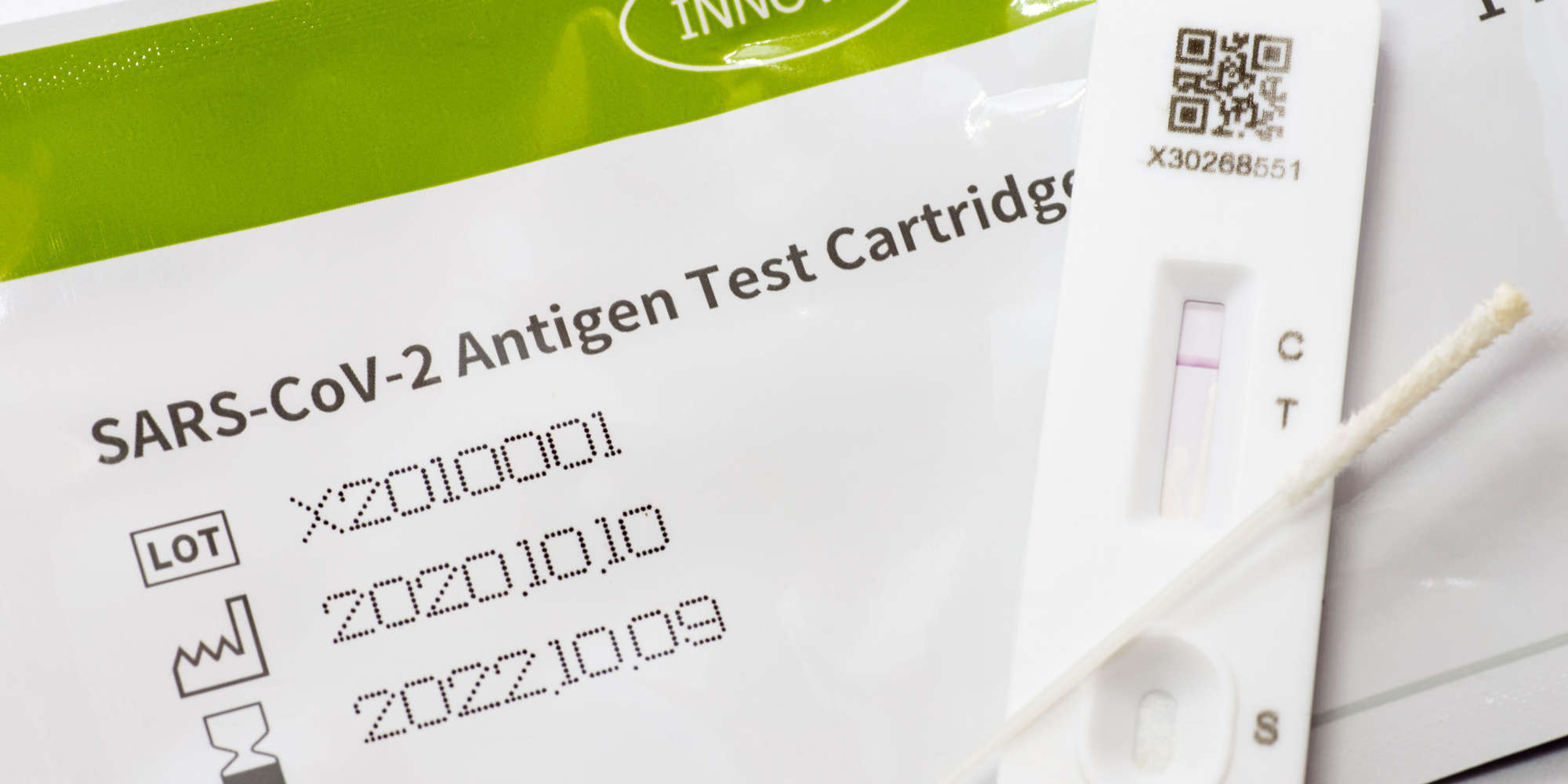
AgPOCTs are small, cheap, portable medical devices that detect a SARS-CoV-2 protein in a patient sample. To use an AgPOCT, a patient sample is placed at one end of a test strip and is wicked to the other end via capillary action. If the sample contains a detectable SARS-CoV-2 protein, a positive result is indicated via the appearance of a line on the device, similar to a pregnancy test.
However, AgPOCTs don’t match the gold standard of lab-based RT-PCR testing in two important measures: sensitivity and specificity. Sensitivity is the ability of a test to correctly identify those with COVID-19, while specificity is its ability to correctly identify healthy individuals — a test with high specificity would have few false positives.
Christian Drosten, of Charité – Universitätsmedizin Berlin, led a collaboration across several German institutes which performed a comparative analysis of the sensitivities and specificities of seven AgPOCTs that had recently become available on the European market. The tests were pitted against a variety of samples, including SARS-CoV-2 protein, respiratory samples known to have SARS-CoV-2 viruses, and samples containing other coronaviruses and respiratory pathogens.
The team found that the AgPOCTs have limits in sensitivity, and noted in their paper that the tests lack the power to provide a definitive diagnosis, especially in very early or later-phase infections. The team noted that most tests showed acceptable specificities, with all but two having a false-positive rate of less than 3%.
Despite falling short of the sensitivity offered by RT-PCR, the sensitivities of most tested AgPOCTs overlapped with the viral loads typically seen in infectious patients, suggesting that AgPOCTs could provide a quick, snapshot assessment of a patient’s infectivity.
The availability of a fast and cheap tool to measure a patient’s infectivity could offer a powerful tool to inform public health decisions, such as having individuals quarantine based on infectivity rather than merely infection. The authors also state that AgPOCTs may find use in hospital environments, for example by enabling clinicians to decide which patients to isolate.
References
Corman, V. M., et al. Comparison of seven commercial SARS-CoV-2 rapid point-of-care antigen tests: a single-centre laboratory evaluation study. Lancet Microbe (2021). | article