26 April 2021
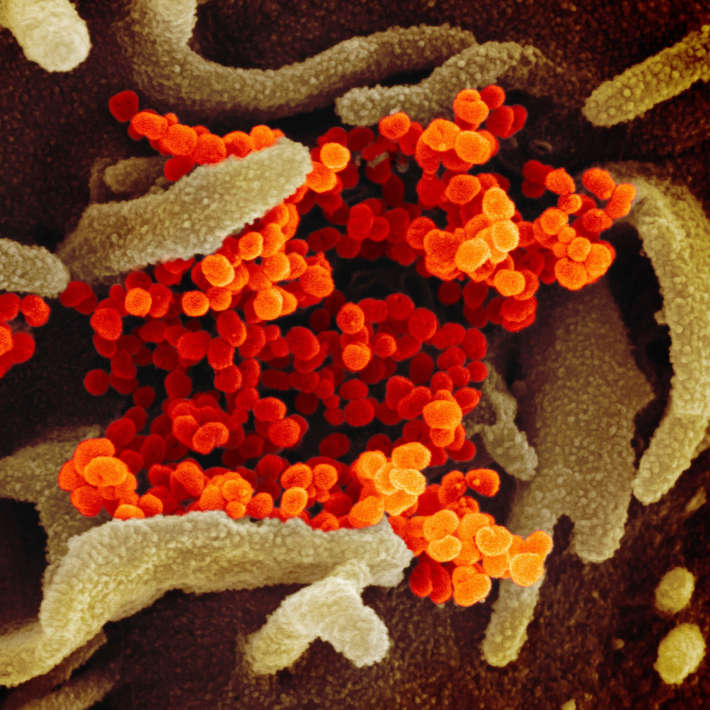
Two new studies1,2 reveal how the body’s innate immune system reacts to a SARS-COV-2 infection in severe and critical cases, which could indicate new treatment trajectories.
The findings show that certain immune defects lead to interferon deficiency, typically worsening prognosis, and that an autoimmune-like antibody response to interferons explains serious infections in some patients. Interferons (IFNs) are proteins that are involved in intercellular signalling and play a role in blocking viral proliferation and modulating the immune response. A lack of the receptors for specific IFNs which provide a defence barrier against viruses and bacteria can make people more susceptible to infectious diseases. The new research demonstrates the critical role played by these antiviral signalling molecules in the immune response to SARS-CoV-2.
The studies were led by Jean-Laurent Casanova and Laurent Abel of the Rockefeller University, in New York, and co-authored by Qian Zhang, Paul Bastard and Lindsey B. Rosen, together with colleagues around the world including Saeed Al Turki of KAIMRC.
In the first study, Zhang and his colleagues sequenced the genomes of 659 patients with life-threatening COVID-19 pneumonia and 534 people with an asymptomatic or mild infection. The scientists examined three IFN-related genes that are mutated in patients with life-threatening influenza pneumonia, along with 10 other genes connected to them.
They found that 3.5% of patients with critical COVID-19 pneumonia had loss-of-function mutations in genes involved in the type I IFN pathway. In other words, these individuals had innate immune errors that would make them more vulnerable to viruses such as SARS-CoV-2. Despite this, none of these patients had been previously hospitalized for other serious viral illnesses, according to Abel.
The second study, led by Bastard, analysed 987 patients who were hospitalized for critical COVID-19 pneumonia, along with 663 with asymptomatic or mild SARS-CoV-2 infections, and samples collected from 1227 healthy control people before the COVID pandemic.
The scientists detected high levels of neutralizing antibodies against type I IFN subgroups in about 10% of patients with COVID-19 pneumonia. These antibodies, which hindered the ability of IFN to fight a SARS-CoV-2 infection, were not found in asymptomatic, mild, or healthy cases, but were present before infection in the patients who developed severe cases.
“The two papers are really two sides of the same coin,” says Bastard. Through a genetic defect in one case and an autoimmune response in the other, the papers demonstrate “two different mechanisms that have the same consequence, which is a defect in this type I interferon.”
Prevalence of hidden defects
Akiko Iwasaki, a professor at Yale School of Medicine who focuses on innate immune defence against viruses and adaptive immunity, calls these results “quite surprising,” particularly the neutralizing antibody response to interferons.
“We know that these kinds of antibodies become prevalent in certain autoimmune conditions,” explains Iwasaki, who was not part of either research team. “But the fact that they are so enriched in patients with severe COVID and that they are functionally blocking interferon would make you just as immunocompromised as if you didn't have the genes for it.”
Casanova and Abel were among a team of scientists who established the COVID Human Genetic Effort3 to understand why SARS-CoV-2 has proven deadly for some patients but has not presented symptoms in others. They hypothesized that severe cases could be related to irregular genetic variations and hidden immunodeficiencies3,4.
The new studies lend support to this idea by showing that genetic defects or autoimmunity underlie many of the severe cases. However, it’s unclear why these factors didn’t cause earlier infections or other problems for the patients.
“The patients with genetic defects did not have any particular symptoms or comorbidity, and most of them didn’t suffer from any severe infections before,” says Bastard. “We haven't really had the chance to analyse all the comorbidities in detail because of the COVID situation. We had a hard time getting access to a complete medical history, but so far it doesn’t seem like there's anything striking about these patients when compared to patients without these genetic or immune defects.”
Like Iwasaki, Paul Hertzog, an immune biology researcher and the associate director of the Hudson Institute of Medical Research, was surprised by the frequency of the defects found in the studies. “It was very surprising because it was much, much more prevalent than what you would normally see in other susceptibilities to infections,” says Hertzog, who was not involved in either study. “This signals that there might be a lot more similar genetic defects yet to be found. There are dozens more genes involved in interferon production and action, so this could be the tip of the iceberg.”
The male bias and the future of therapy
Understanding the physiology of the severe cases and why a breakdown in the antiviral interferon system happens can open avenues of prevention and early intervention. For instance, patients who cannot produce interferon can be treated using synthetic interferons. “You can very easily give recombinant type I interferon, either IFN alpha or beta, but the really important point is to give it early in the disease,” says Bastard. He adds that patients with IFN alpha auto-antibodies could be treated by giving them IFN beta, which wouldn’t be inhibited by the antibodies because it has a different structure.
Abel concurs. “Having this information for at-risk patients, especially those who haven’t yet developed a severe form, is very important,” he says. “The treatment by interferon is efficient when given at a very early stage of infection. If the person is already hospitalized with a severe form, then it’s likely to be too late.”
The findings also have broader implications for therapeutics. For example, both Abel and Bastard point out the need to test all convalescent plasma donated to sick patients to ensure that it is free of IFN-neutralizing auto-antibodies which could make the disease.
Hertzog also points out that “together, the patients from the studies probably represent close to 15% of seriously ill people [who] can't respond to interferon, the body's best natural defence against the virus.” That's a significant number of people might not respond to therapeutics that work for the rest of the population.
The IFN antibodies may also explain why older males are among the most vulnerable demographic. The neutralizing auto-antibodies were mostly found in older males— 95 of the 101 patients with these antibodies were men. Abel says that it isn’t enough to explain general male susceptibility to severe COVID-19, but it’s certainly part of the story.
He and his colleagues plan to build on this by investigating the genetic basis of these auto-antibodies and the reasons for the male bias. “We need to know why these individuals develop auto-antibodies, and if it’s, for example, somehow related to the X-chromosome,” he explains. The researchers also want to replicate their findings and test them more broadly to see if they hold in less milder cases of COVID-19 or other viral diseases.
References
- Zhang, Q., et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science 370, 422 (2020) | article
- Bastard, P. et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science 370, 423 (2020) | article
- Casanova, J.L., et al. A Global Effort to Define the Human Genetics of Protective Immunity to SARS-CoV-2 Infection. Cell 181, 1194-1199 (2020) | article
- Casanova, J.L., Abel, L. Lethal Infectious Diseases as Inborn Errors of Immunity: Toward a Synthesis of the Germ and Genetic Theories. Annual Review of Pathology: Mechanisms of Disease 16 (2020) | article