11 February 2019
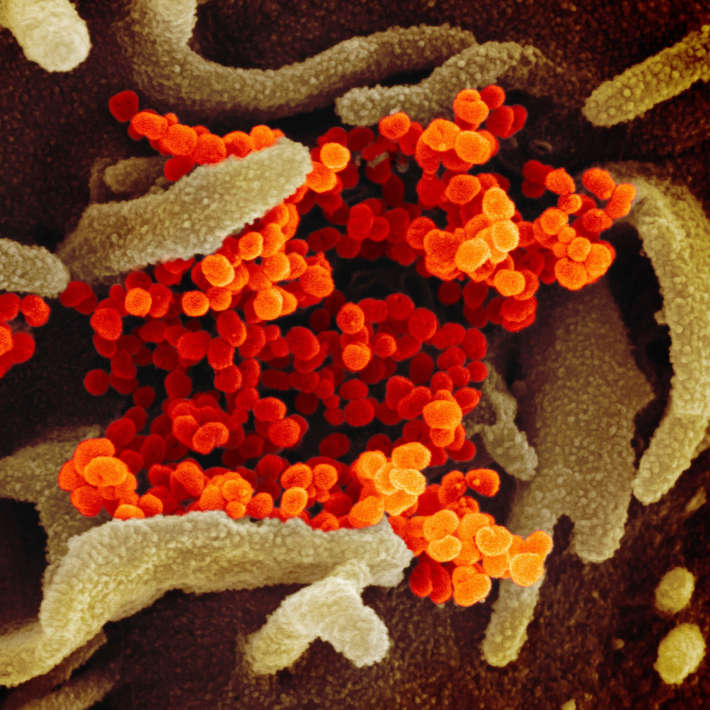
Bacterial blood infections, many of which are contracted in hospitals, are a leading cause of disease and death worldwide. Gram-negative bacteria, such as pathogenic Escherichia coli (E. coli), are becoming increasingly resistant to firstline antibiotics, presenting significant challenges in tackling infections.
Faisal AlMajed and co-workers at King Saud Bin Abdulaziz University for Health Sciences in Riyadh investigated E. coli susceptibility to different drugs over the course of a year. Their results have implications for the treatment of men and women of different ages through different seasons.
“Information regarding bacterial infection, bacteraemia, and antimicrobial resistance in Saudi Arabia is scarce,” says AlMajed. “We wanted to find out more about E. coli in our hospital to improve understanding of currently circulating bacteria and potentially help tackle infections more successfully.”
AlMajed’s team took blood samples from 181 E. coli-infected patients of all ages at King Abdulaziz Medical City’s King Fahd Hospital in the period from January to December 2013. 174 of the isolates were from patients who contracted the infection in hospital. They found that the E. coli isolates were least sensitive to ampicillin, a widely used broad-spectrum antibiotic. The bacterial isolates were most sensitive to amikacin, with sensitivity to this drug peaking in June and September. AlMajed’s team found several other drugs that worked effectively in other months of the year.
Patients’ ages impacted drug sensitivity, with 94.9% of patients over 70 responding well to the antibiotic amikacin. E. coli in younger patients, aged 20 to 45 years, proved highly susceptible to ciproflaxin. The researchers also observed differences in drug sensitivity dependant on the sex of the patient, with females responding better to ciproflaxin and tobramycin.
Bacteria can evade antibiotics by producing enzymes known as extended-spectrum beta-lactamases (ESBLs). These enzymes break the internal structure of the antibiotic molecule, destroying its antibacterial properties and enabling bacteria to survive multiple drug types. Interestingly, despite other studies finding that ESBL-producing bacteria are on the rise, AlMajed’s team found that non-ESBL-producing E. coli species increased at the hospital by 12.2% over the course of the year, particularly in patients aged 46 to 76. They caution this result may not reflect patterns across the wider community, being a finding from a single hospital.
The team’s insights could help authorities and clinicians manage patients with bacterial blood infection more carefully. Their results provide further evidence indicating a worrying trend of proliferating strains that are resistant to first-line antibiotics in the region.
References
- AlMajed, F., Swailem, Y.B.S., AlJaser, F., Aqel, H., Al-Juhani, S. & Qureshi, S. Antimicrobial susceptibility of Escherichia coli isolates from blood in relation to age, sex and months. International Educational Scientific Research Journal (2017). | article