11 February 2019
Just under a third of hepatitis patients surveyed at King Abdulaziz Medical City in Riyadh did not attend a follow-up appointment with the hospital. More than two-thirds of those weren’t aware an appointment had been scheduled. Researchers urge better information, education and communication to help reduce the incidence of liver disease complications.
Minimising the number of patients who become unreachable — known in the medical field as ‘lost to follow-up’ — during treatment programmes is critical. For people with hepatitis, insufficient care can lead to serious complications such as liver scarring (cirrhosis), failure and cancer.
Close to 400 million people are affected by the hepatitis B virus (HBV) and another 170 million are living with hepatitis C virus (HCV) around the world. In Saudi Arabia, despite a large-scale HBV vaccination initiative launched in 1989, the incidence of both types of the disease remains higher than expected.
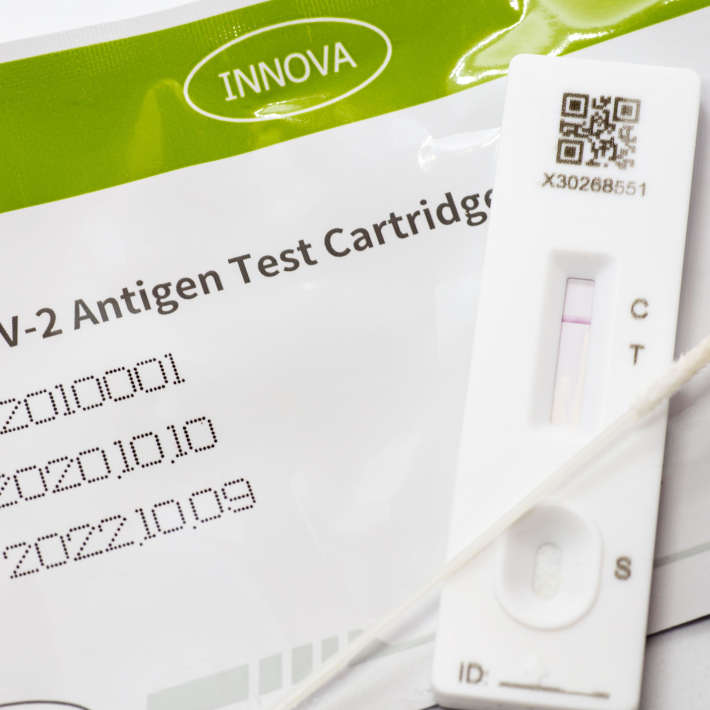
To gain a better idea of the number of hepatitis patients who drop out of treatment, and to reveal the reasons behind the lack of follow-up, a multi-institutional team surveyed people diagnosed with HBV and HCV between 2009 and 2010 at King Abdulaziz Medical City (KAMC) in Riyadh.
The team was led by Hanan Balkhy, chairman of KAIMRC’s infectious disease section and executive director of the Infection Prevention and Control Program at the Ministry of National Guard– Health Affairs (NGHA). Of a total of 328 patients who completed the telephone survey, 98 (around 30%) were deemed lost to follow-up.
Of those 98, the top reason given (by 69% of respondents) for not returning for treatment was that they were unaware that a follow-up appointment was scheduled. Other reasons given were that they were never informed about the need for follow-up (15%) or they had a personal belief that follow-up was not necessary (9%).
The number of patients lost to follow-up was found to be higher among those diagnosed with HBV (71.4%) compared with HCV (28.6%). As yet, the full extent of the problem nationwide is unknown. Since the study was conducted at just one large NGHA-affiliated hospital, the researchers point out that “the reported 30% may underestimate the magnitude of the problem at primary care centres and at the community level, where many people have never been diagnosed or referred.”
If left undiagnosed or untreated, the burden of liver disease on hospitals and families will continue to increase and lead to a greater number of people requiring transplants.
The study calls for a greater focus on education, as well as more efficient and flexible referral and scheduling systems. A dedicated health centre for hepatitis patients may help achieve this goal. The team suggests that sending reminders to patients via text messaging and email will also be important.
References
- Balkhy, H. H., El-Saed, A., Sanai, F. M., Alqahtani, M., Alonaizi, M. et al. Magnitude and causes of loss to follow-up among patients with viral hepatitis at a tertiary care hospital in Saudi Arabia. Journal of Infection and Public Health 10, 379—387 (2017). | article