18 February 2021
Nearly half of cancer patients don’t complete their full course of treatment. Multiple hospital trips, invasive procedures, and repeated physical and psychological distress all affect the ability of patients to persist with life-saving therapies. A US-developed drug delivery system looks to alleviate some of this burden by packaging a cancer therapy within micro-sized cubes that are able to deliver a weeks-long course of cancer treatments from a single injection.
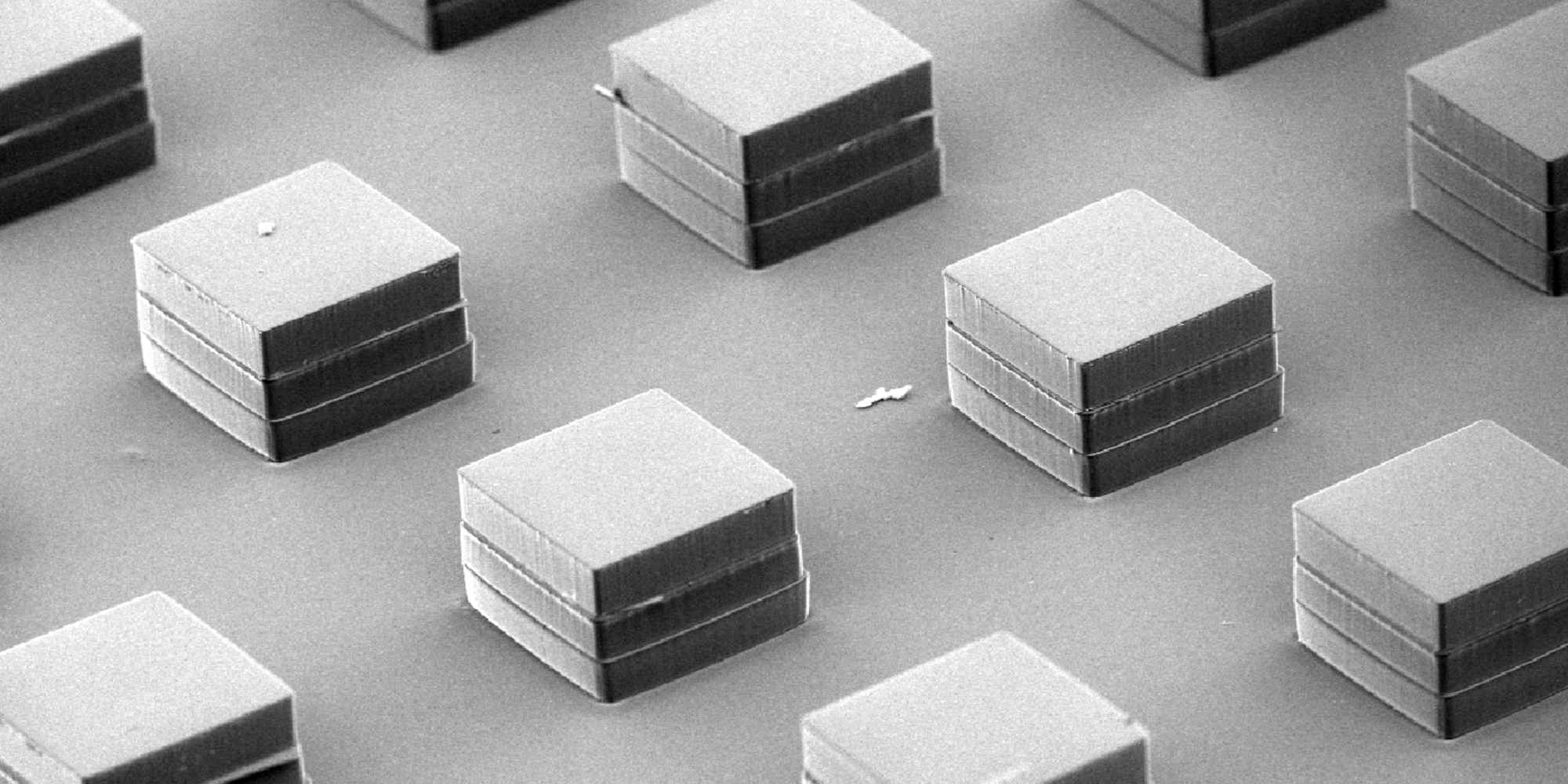
Led by researchers at the Massachusetts Institute of Technology (MIT), the team behind the new development constructed hollow microcubes of a material called polylactic-co-glycolic acid (PLGA), measuring less than half a millimeter per side. In contrast to existing slow-release drug delivery systems, these microparticles release their payloads in a way “similar to how an egg cracks,” says MIT’s Ana Jaklenec, one of the research team’s leaders.
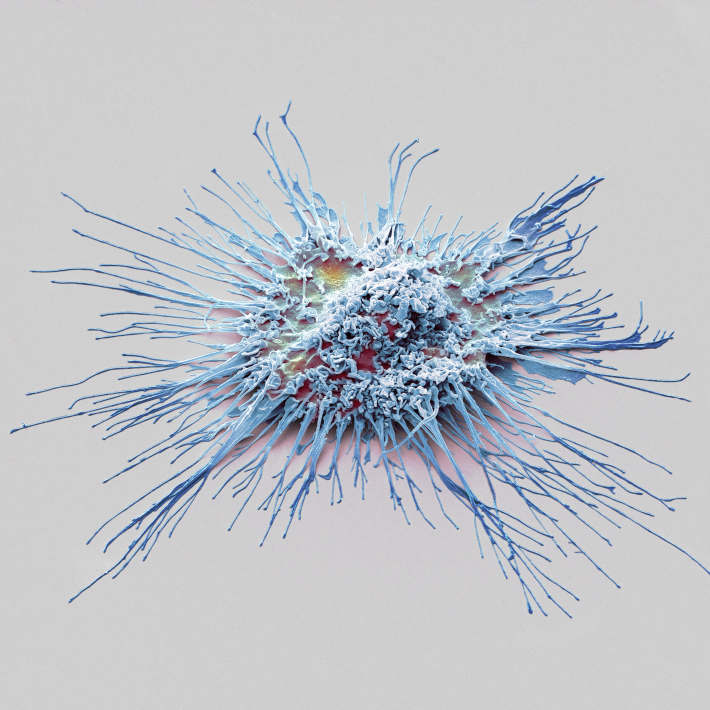
The team designed the PLGA microparticles to be used with the experimental stimulator of interferon genes (STING) agonist cancer therapy, which is being tested in multiple US clinical trials. Currently, the therapy depends on multiple injections directly into a tumor.
The team’s system offers a preferable alternative. By incorporating differently-tuned PLGA cubes into a single injectable solution, the system provides multiple doses over a course of time as the cubes break down sequentially.
The researchers tested the efficacy of their system on mouse models of multiple cancers, including breast cancer, melanoma, and pancreatic cancer. The results showed that a single injection of STING agonist-loaded cubes was able to induce a strong anti-tumor response and effectively inhibit tumor growth both locally and systemically. The treatment was as effective as multiple injections given over time. When injected after the removal of a tumor, the encapsulated STING agonist lowered the chances of recurrence from 100% to 25%.
A critical advantage of a one-shot treatment course is that the tumor and its blood vessels are not repeatedly physically disturbed — this reduces the chances of metastasis, an effect observed by the team in their own study.
The team’s research is set to make STING agonist therapy more bearable and more effective, as well as expanding its scope to more difficult-to-reach tumors. Jaklenec says that her team overcame “several technical challenges” during their research that required them to develop new fabrication methods, in vivo assays, and injection methods.
After optimizing their microparticles and scaling up production, the team hopes to collaborate with pharmaceutical companies to bring their platform to clinical trial.
References
- Lu, X., et al. Engineered PLGA microparticles for long-term, pulsatile release of STING agonist for cancer immunotherapy. Science Translational Medicine 12, eaaz6606 (2020). | article