29 July 2021
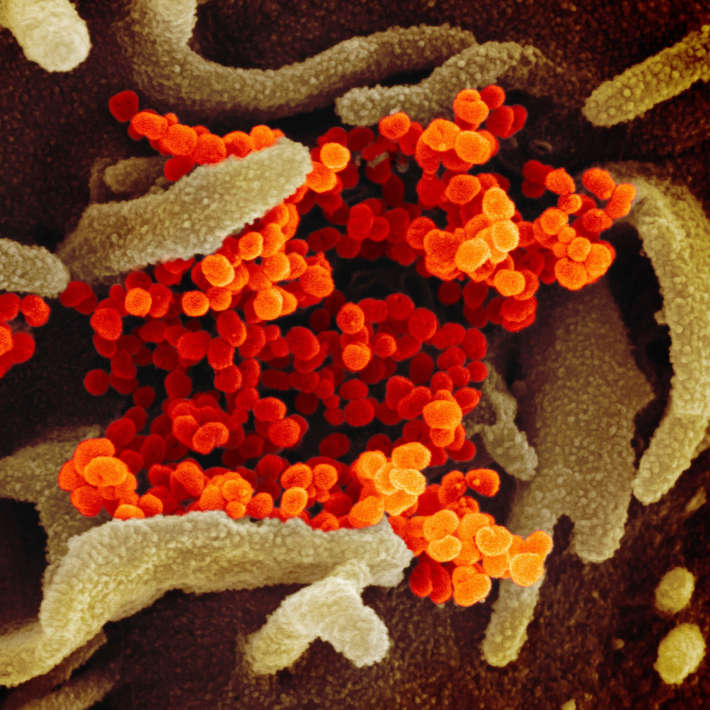
The significant differences in COVID-19 outcomes between humans and animal models mean that different models should be used depending on the questions asked, say KAIMRC researchers. They also propose that genetic engineering might create more accurate models to assist research efforts.
The authors analysed 27 original research papers from January 1 to May 20, 2020. using a variety of primate species, mice, ferrets, and hamsters as models of the human disease. They hoped to identify one or more animal models that effectively mimicked the full range of consequences of COVID-19 in humans.
“Our findings were not what we hoped for,” says Salleh Ehaideb of KAIMRC, explaining that the variety of outcomes in humans was poorly replicated by the model systems. The animal models tended to replicate mild cases of COVID-19 with full recovery phenotype, while researchers aim to help develop therapy and assess vaccines for human that prevent severe disease and fatality.
“We were not surprised by this disappointing finding,” Ehaideb adds, “as studies of other viruses in the same family reached similar conclusions.”
However, the response of animals to experimental vaccines and anti-viral drugs more closely matched the desired response in humans, so they may nevertheless be valuable for proof-of-concept drug trials.
The authors suggest that one reason for the mismatch may be that the virus binds tightly to the ACE-2 receptor on human cells, but less well to the structurally different ACE-2 receptors in animals, particularly rodents, which are the most common laboratory animals.
They also note that although the virus binds well to the ACE-2 receptor of nonhuman primates, which is similar to the human ACE-2 receptor, the animals do not develop severe COVID-19 or die. This is partly because ACE-2 and other receptors which are essential for entry and spread of the virus differ in the lungs, liver, and kidney between human and primates. “This changes the types of tissues and organs that will be severely infected,” says Ehaideb. Another likely factor is significant differences in the immune response in humans and animal models.
This work could help guide other researchers in choosing the best animal model, with its advantages and limitations, for their research, as well as helping clinicians interpret the effects of drugs or vaccines before applying them to humans. Genetic engineering, may also help make the models closer to humans although this might be difficult for coronavirus studies. The KAIMRC team does not have the approved biosafety facilities to develop new models, but they hope other researchers will follow up on their findings and suggestions.
References
- Ehaideb, S. N., et al. Evidence of a wide gap between COVID-19 in humans and animal models: a systematic review. Critical Care 24, Article number: 594 (2020) | article