5 August 2021
A new nanomedicine strategy for delivering drugs to the female reproductive tract could help prevent women from going into labour prematurely.
Each year, around 1 in 10 babies worldwide are born before 37 weeks of gestation, resulting in more than 1 million deaths due to complications resulting from preterm birth. The steroid hormone progesterone is sometimes used to prevent early delivery in at-risk women, but current treatment formulations often have little effect because they fail to deliver the hormone to the appropriate tissues of the cervix and uterus.
A team from Johns Hopkins University in the USA, designed a nanosuspension system that enables vaginally dosed drugs to overcome the mucus barrier of the female reproductive tract and reach uterine tissues, where they can forestall labour.
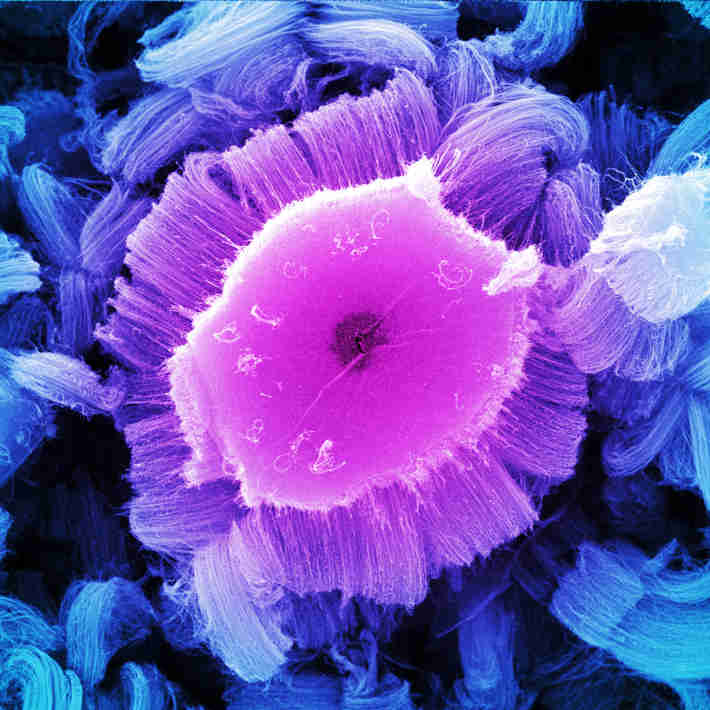
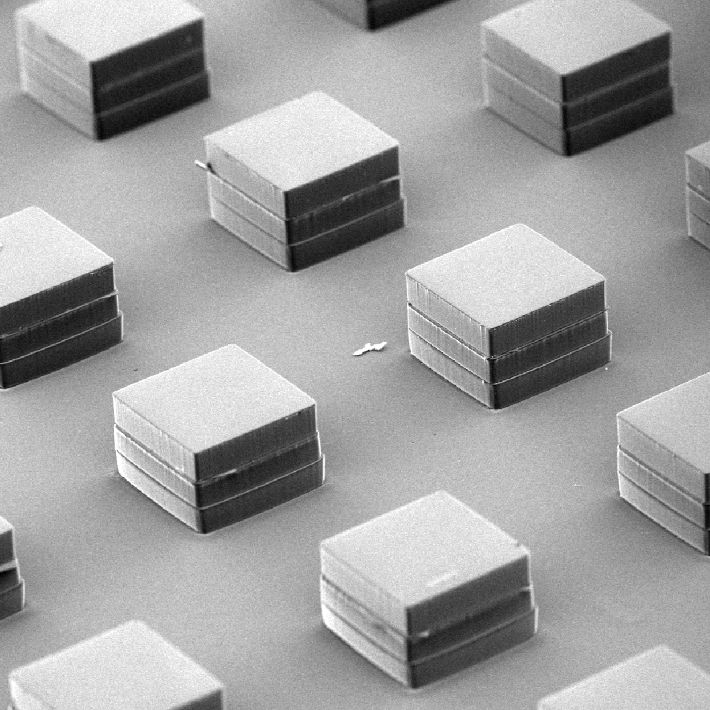
The system involves grinding drugs into miniature crystals about 200–300 nanometers in diameter — smaller than the size of a typical bacterium. A stabilizing agent is then added to keep the nanoparticles from getting stuck in the vagina’s protective mucus, which normally traps foreign particles such as microbes — but also medicines — and prevents their entry into the body.
The researchers tested the system in mice experimentally induced to develop uterine inflammation, an unpredictable major condition that often leads to premature labour in humans and results in nearly 4 million global premature births annually. They focused on vaginal administration of two types of drugs: histone deacetylase (HDAC) inhibitors, which they showed can help to inhibit the contractility of the uterine wall in human cell experiments, and progesterone, which has known anti-inflammatory effects.
The researchers found that mice treated with mucus-penetrating nanosuspensions of HDAC inhibitors, both with and without progesterone, showed improved rates of full-term delivery. Large litters of healthy, normal pups were born. By comparison, mice injected with the drugs in their body cavity — like untreated mice — went into labour prematurely, with no surviving offspring.
“Delivery matters,” says Laura Ensign of Johns Hopkins, who led the research. “And we must sometimes think outside the box of pills and injections to develop effective treatments.”
In other mouse studies, Ensign and her colleagues have used their nanosuspension system to enhance drug delivery in the gut, in the airways and at other mucosal surfaces. Kala Pharmaceuticals, a company cofounded by Ensign’s close collaborator and mentor, Justin Hanes, has licensed the technology and developed two topical eye treatments for people, one for dry eye disease and one for post-operative ocular inflammation and pain.
“There are many diseases affecting mucosal surfaces that would benefit from more targeted local and sustained drug delivery,” Ensign says. Fortunately, her technology now makes that possible.
References
Zierden, H.C. et al. Enhanced drug delivery to the reproductive tract using nanomedicine reveals therapeutic options for prevention of preterm birth. Science Translational Medicine 13, eabc6245 (2021).
| article